Lancet Oncol:奥拉帕利长期维持治疗对患者生活质量的影响
2021-04-25 MedSci原创 MedSci原创
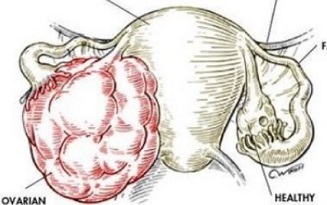
在3期SOLO1试验中,奥拉帕利维持治疗为新确诊的携带BRCA突变的经以铂类为基础的化疗后获得缓解的晚期卵巢癌患者提供了相比安慰剂组明显延长的无进展生存期益处。
在3期SOLO1试验中,奥拉帕利维持治疗为新确诊的携带BRCA突变的经以铂类为基础的化疗后获得缓解的晚期卵巢癌患者提供了相比安慰剂组明显延长的无进展生存期益处。
本文分析了SOLO1试验患者的健康相关生活质量(HRQOL)和以患者为中心的预后分析结果,以及放射疾病进展对健康状况的影响。
SOLO1试验是一项在15个国家118个中心开展的随机、双盲的3期试验,招募了年满18岁的ECOG表现状态评分0-1分新确诊的携带BRCA突变的晚期高级别浆液性或内膜样卵巢癌、原发性腹膜癌或输卵管癌患者。受试患者被随机(2:1)分至奥拉帕利(300 mg,2/日,口服)组或安慰剂组。HRQOL(TOI评分)是次要终点。
2013年9月3日-2015年3月6日,共招募了1084位患者,其中693位符合要求,最终260位患者被分至奥拉帕利组、131位患者被分至安慰剂组。
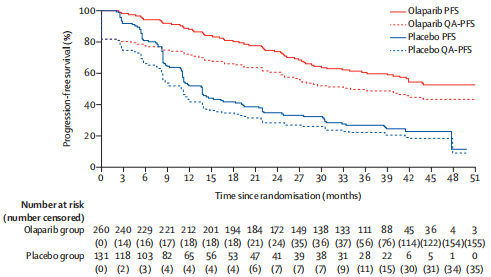
两组的PFS和经生活质量校正的PFS
奥拉帕利组和安慰剂组的中位随访时间分别是40.7个月和41.2个月。24个月时,两组的TOI评分均无临床显著意义的改变(从基线到24月时校正平均评分变化分别是0.3分[奥拉帕利组] vs 3.30分[安慰剂组];组间差异-3.0,95% CI -4.78~-1.22;p=0.0010)。奥拉帕利组生活质量校正的无进展存活期(平均值:29.75个月 vs 17.58个月;差值 12.17个月,p<0.0001)和TWiST平均持续时间(33.15个月 vs 202.24个月;差值 12.92个月,p<0.0001)均显著长于安慰剂组。
综上所述,对于该试验评估的癌症类型患者,奥拉帕利维持治疗不仅可以提供优秀的无进展存活期益处,而且不会降低患者的生活质量。
原始出处:
Michael Friedlander, et al. Atezolizumab, Bevacizumab, and Chemotherapy for Newly Diagnosed Stage III or IV Ovarian Cancer: Placebo-Controlled Randomized Phase III Trial (IMagyn050/GOG 3015/ENGOT-OV39). The Lancet Oncology. April 13, 2021. https://doi.org/10.1016/S1470-2045(21)00098-X
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Oncol#
26
#Lancet#
0
#Lancet oncol# 点击看更多,点我头像关注更多福利
80
顶刊就是不一样,质量很高,内容精彩!学到很多
44
谢谢梅斯分享这么多精彩信息
60