Euro Radiol:深度学习在冠状动脉斑块风险分层中的应用
2022-08-03 shaosai MedSci原创
深度学习方法发展迅速,在医学影像分析中表现出良好的泛化能力和高效率。
 冠状动脉疾病(CAD)是世界范围内造成死亡的主要原因,其中动脉粥样硬化斑块在CAD相关患者的死亡中起着决定性。因此,冠状动脉斑块的识别和分类对于CAD的早期预防和干预具有重要的临床意义。冠状动脉计算机断层扫描(CTA)是检测冠状动脉狭窄和表征斑块成分的一种重要的成像方式。在临床实践中,冠状动脉斑块的诊断主要是通过耗时的手工操作进行的,这取决于临床医生的经验和对图像的主观视觉判析。
冠状动脉疾病(CAD)是世界范围内造成死亡的主要原因,其中动脉粥样硬化斑块在CAD相关患者的死亡中起着决定性。因此,冠状动脉斑块的识别和分类对于CAD的早期预防和干预具有重要的临床意义。冠状动脉计算机断层扫描(CTA)是检测冠状动脉狭窄和表征斑块成分的一种重要的成像方式。在临床实践中,冠状动脉斑块的诊断主要是通过耗时的手工操作进行的,这取决于临床医生的经验和对图像的主观视觉判析。
为了将放射科医生从繁琐的工作中解放出来,人们提出了许多自动计算机辅助方法来对CTA图像进行后处理。最近,深度学习方法发展迅速,在医学影像分析中表现出良好的泛化能力和高效率。然而,深度学习方法在医学应用中的一个主要缺点是可解释性有限,这意味着神经网络就像一个 "黑匣子",放射科医生只能看到它的输出结果而不知道它是如何工作的。放射组学是一种新兴的影像分析工具,可通过提取数据的高通量信息以改善诊断和预测预后。
近日,发表在European Radiology杂志的一项研究开发了一个同时使用深度学习和放射组学方法的自动系统来分割冠状动脉、检测斑块并进行分类以及对狭窄进行分级,为减少放射科医生的图像阅读时间、提供较高的冠状动脉斑块和狭窄分析精度提供了技术支持。
本项研究回顾性地纳入了505名患者,共有127763张来自5个医疗中心的计算机断层扫描血管成像(CTA)图像。使用卷积神经网络(CNN)模型对冠状动脉进行分割以检测斑块候选者,并以高计算效率提取图像信息。利用人工设计的放射组学特征提取器来收集斑块模式,然后用不同的分类器来进行斑块分类和狭窄程度分级。
与U-Net和基线模型相比,CNN模型在斑块候选检测中取得了100%的灵敏度和最高的阳性预测值(83.9%)。选择了26个代表性的放射组学特征来构建分类器。在不同的模型中,梯度增强决策树(GBDT)在斑块分类(准确率:87.0%,灵敏度:83.2%,特异性:91.4%)和狭窄分级(准确率:90.9%,灵敏度:84.1%,特异性:95.7%)方面取得了最佳性能。GBDT在斑块分类中也达到了最高的AUC,为0.873,在狭窄分级中为0.910。处理一名患者的计算时间为56.2±5.7秒,明显低于放射科医生的人工分析(285.6±134.5秒,P=0.0001)。
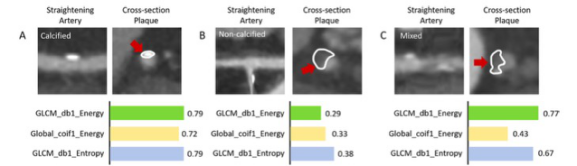
图 三种类型典型斑块的代表性图像。(A)钙化的,(B)非钙化的,和(C)有三种放射组学特征的混合型。每种类型的斑块都有不同的特征值,表现出不同的模式。红色箭头表示冠状动脉中的斑块,白色轮廓表示进行放射组学分析的区域
本研究提出了一个自动检测和分析冠状动脉斑块的工作流程,利用深度学习和放射组学方法的优势实现了斑块检测、分类和狭窄分级的高准确性和高效率,为临床提供了一个可靠的进行患者风险分层的影像学工具。
原文出处:
Xin Jin,Yuze Li,Fei Yan,et al.Automatic coronary plaque detection, classification, and stenosis grading using deep learning and radiomics on computed tomography angiography images: a multi-center multi-vendor study.DOI:10.1007/s00330-022-08664-z
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#冠状动脉斑块#
45
#斑块#
35
#风险分层#
45
认真学习~~
35