Lung Cancer:安罗替尼可改善晚期非小细胞肺癌患者的生活质量
2018-05-31 佚名 肿瘤资讯
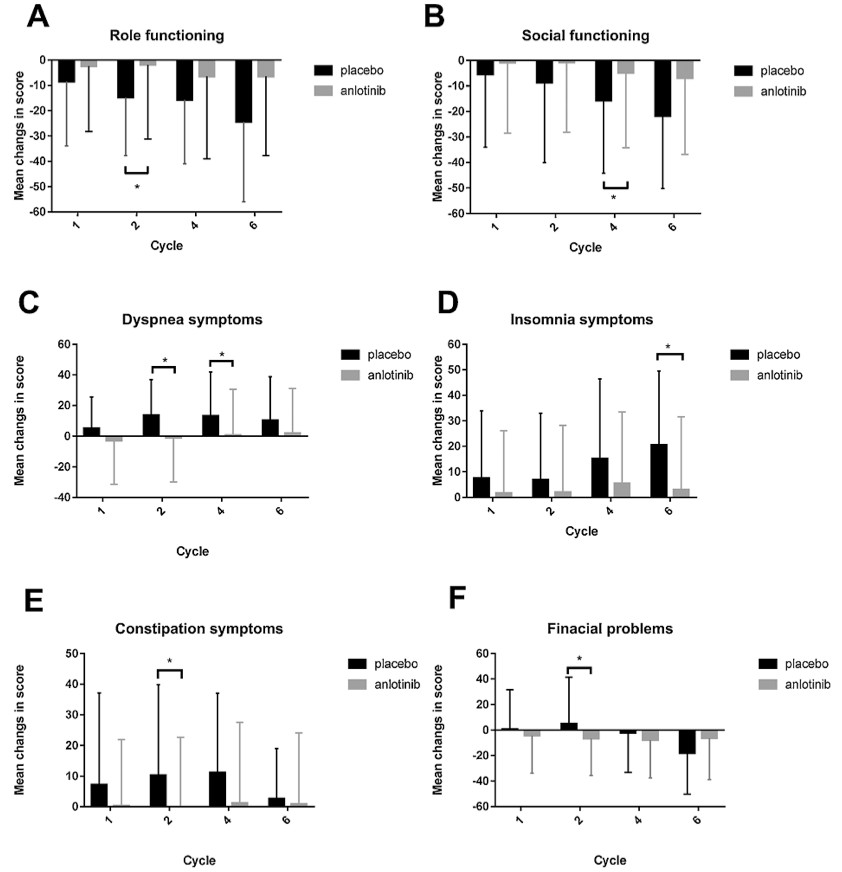
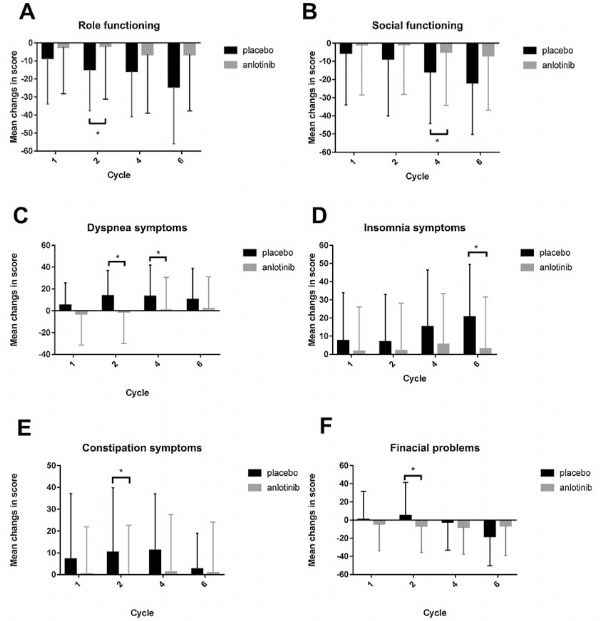
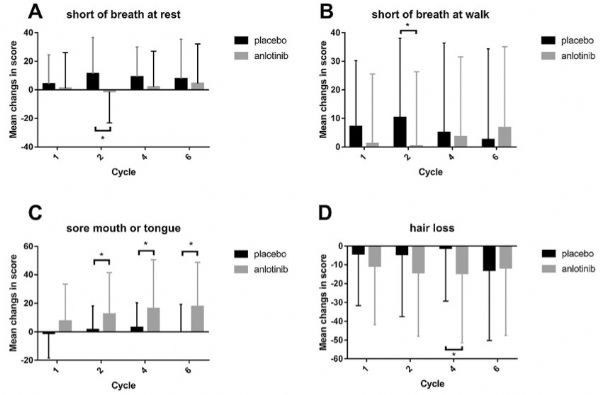
目前,晚期NSCLC患者的三线治疗尚无标准方案,ALTER-0303试验已经证实安罗替尼在三线及以上治疗晚期NSCLC患者的有效性和安全性。北京协和医院的张力教授团队在前期研究的基础上,对接受安罗替尼治疗的患者的生活质量进行了研究,结果显示,除了口疮或舌头症状外,安罗替尼在其他方面都比安慰剂更佳。其结果于5月17日发表于著名肺癌研究杂志《Lung Cancer》上。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#肺癌患者#
38
#非小细胞#
30
#非小细胞肺癌患者#
34
学习
78
阅
70
学习学习.继续关注
60
学习.谢谢分享
56
学习学习再学习
59
一起学习学习
0