J Clin Oncol:中山大学附属肿瘤医院石明教授团队随机试验证实,采用FOLFOX进行肝动脉灌注化疗可显著延长不可切除的大肝癌患者的生存期!
2021-10-17 Nebula MedSci原创
采用氟尿嘧啶、亚叶酸和奥沙利铂进行肝动脉灌注化疗与经动脉化疗栓塞相比可显著延长不可切除的大肝癌患者的总生存期
在一项既往II期临床试验中,采用氟尿嘧啶、亚叶酸和奥沙利铂(FOLFOX)进行肝动脉灌注化疗(HAIC)在不可切除的大肝细胞癌中产生了比经动脉化疗栓塞(TACE)更高的治疗反应。
中山大学附属肿瘤医院肝肿瘤科石明主任率团队开展了一项随机、多中心、开放标签的临床试验,旨在比较使用 FOLFOX-HAIC 或 TACE 作为一线治疗的不可切除的大肝癌(肿瘤直径≥7cm)患者的总生存期。
不可切除的大肝癌患者被1:1随机分至 FOLFOX-HAIC组(第1天灌注奥沙利铂 130 mg/m2、亚叶酸 400 mg/m2和氟尿嘧啶 400 mg/m2,再输注氟尿嘧啶 2400 mg/m2,持续24 小时,每3周一疗程) 或 TACE 组(表柔比星 50 mg、洛铂 50 mg、碘油和聚乙烯醇颗粒)。主要终点是意向治疗分析中的总生存期。在接受≥ 1 个研究治疗疗程的患者中评估安全性。
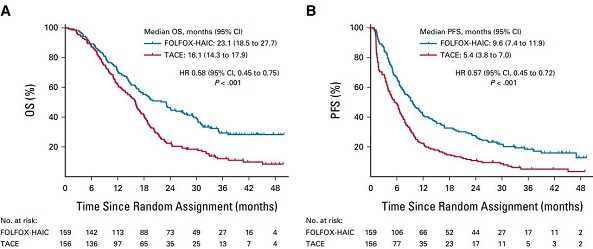
两组的总生存期和无进展生存期
自2016年10月1日至2018年11月23日,共有315位患者被随机分至FOLFOX-HAIC 组(n=159)或 TACE 组(n=156)。FOLFOX-HAIC 组和TACE 组的中位总生存期分别是23.1个月(95% CI 18.5-27.7)和16.1个月(95% CI 14.3-17.9; 风险比 0.58. 95% CI 0.45-0.75; P<0.001)。与 TACE 组相比,FOLFOX-HAIC 组表现出明显更高的缓解率(46% vs 18%; P<0.001)和更长的无进展生存期(9.6 vs 5.4个月;P<0.001)。
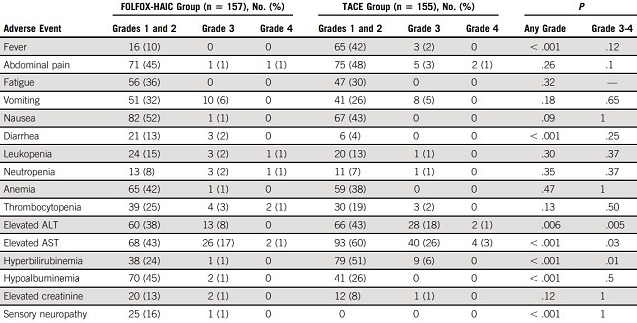
两组的不良反应事件发生情况
除此之外,TACE 组的严重不良反应事件的发生率高于 FOLFOX-HAIC 组(30% vs 19%;P=0.03)。FOLFOX-HAIC 组和 TACE 组各有两例死亡被认定与治疗相关。
总而言之,FOLFOX-HAIC 治疗方法与 TACE 相比可显著延长不可切除的大肝癌患者的总生存期。
原始出处:
Qi-Jiong Li, et al. Hepatic Arterial Infusion of Oxaliplatin, Fluorouracil, and Leucovorin Versus Transarterial Chemoembolization for Large Hepatocellular Carcinoma: A Randomized Phase III Trial. Journal of Clinical Oncology. October 14, 2021. https://ascopubs.org/doi/full/10.1200/JCO.21.00608
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#肝癌患者#
43
#肿瘤医院#
34
#Oncol#
21
#生存期#
30
#FOLFOX#
27
#随机试验#
41
#中山大学#
38
赞
56
这个厉害,将#肝癌#的OS从16个月提升至23个月!象这种情况,对于大肝癌,局部用消融减负荷,然后再用肝动脉灌注化疗,会不会可能更好??
134