BMJ:心脏复律可降低新诊断非瓣膜性房颤患者不良预后风险
2021-10-28 MedSci原创 MedSci原创
对于新发病的非瓣膜性房颤患者,仅有一小部分患者接受了心脏复律治疗,其中大部分选择了直流电复律。研究发现,复律方式对患者预后无显著影响,但心脏复律组死亡率明显低于非复律组

临床上房颤的治疗方法有两种,一种方法是尝试恢复窦性心律,即节率控制,可以通过电击或药物实现,该方法可缓解症状,预防房颤和左心房重构;另一种治疗选择是控制心率。有研究发现,以卒中率和死亡率为终点时,控制心率的临床效果与节律控制相当;若以住院率为终点时,控制心率的临床效果优于节律控制。近日,研究人员在近期发病的非瓣膜性房颤患者中,比较了心率和节率控制对患者临床结果的影响。
FIELD-AF-GARFELD-AF研究在35个国家的1317个医疗中心开展,52057名年龄在18岁及以上的新诊断房颤患者(持续时间长达6周)参与,患者存在至少一种中风风险因素。根据基线检查时是否接受心脏复律分组。在复律组中,比较电击复律和药物复律患者的预后差异,主要终点事件包括全因死亡率、非出血性卒中或系统性栓塞、大出血。
筛查后,总计44201名患者纳入终点分析,其中6595名(14.9%)患者接受了心脏复律。随访1年后,与心率控制组相比,心脏复律组全因死亡率的倾向评分加权危险比为0.74,在1-2年随访期间,心脏复律组全因死亡率的倾向评分加权危险比为0.77。在基线检查时接受了心脏复律治疗的6595名患者中,299名在基线后至少48天接受了后续心脏复律治疗。7175接受心脏复律的患者中,2427名(33.8%)接受药物复律,4748名(66.2%)接受电击心脏复律。在一年的随访期间,接受直流电和药物心脏复律的患者全因死亡事件发生率为每100患者随访年1.36和1.70例。
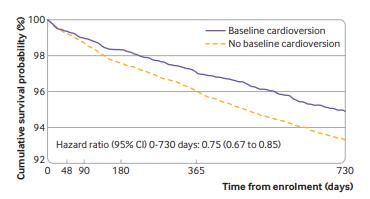
复律组预后显著提高
对于新发病的非瓣膜性房颤患者,仅有一小部分患者接受了心脏复律治疗,其中大部分选择了直流电复律。研究发现,复律方式对患者预后无显著影响,但心脏复律组死亡率明显低于非复律组。
原始出处:
Marita Knudsen Pope et al. Cardioversion in patients with newly diagnosed non-valvular atrial fibrillation: observational study using prospectively collected registry data.BMJ. 27 October, 2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#非瓣膜性#
58
#心脏复律#
38
#非瓣膜性房颤患者#
46
#瓣膜性#
42
#新诊断#
38
#非瓣膜性房颤#
40
#BMJ#
0
#不良预后#
36
#瓣膜#
28
#房颤患者#
30