J Clin Invest:研究揭开了IFN-γ介导的肠道血管激活在IBD中的致病影响
2020-09-28 MedSci原创 MedSci原创
炎症性肠病(IBD)是一种慢性炎症性疾病,发病率不断上升。病变组织有大量的血管,然而血管在IBD中的致病影响和潜在的调节机制尚未可知,研究结果已在线发表于J Clin Invest。
炎症性肠病(IBD)是一种慢性炎症性疾病,发病率不断上升。病变组织有大量的血管,然而血管在IBD中的致病影响和潜在的调节机制尚未可知,研究结果已在线发表于J Clin Invest。
IFN-γ是IBD发病过程中的主要细胞因子,但在该病的背景下,人们考虑的几乎只是其免疫调节和上皮细胞导向功能。我们小组最近的研究表明,IFN-γ对血管也有强大的作用。基于这些考虑,我们分析了IFN-γ的血管导向致病功能,发现其通过破坏血管屏障来驱动IBD的发病。
具体来说,我们表明,通过内皮特异性敲除IFN-γ受体2抑制血管中的IFN-γ反应,可以改善实验诱导的小鼠结肠炎。IFN-γ通过破坏粘连结蛋白VE-cadherin,导致血管屏障的破坏,从而起到致病作用。值得注意的是,在人类IBD患者中也证实了肠道血管屏障功能障碍,支持我们的研究结果的临床意义。使用伊马替尼治疗可以恢复VE-cadherin/adherens交界,抑制血管通透性,并显著降低实验性结肠炎的结肠炎症。
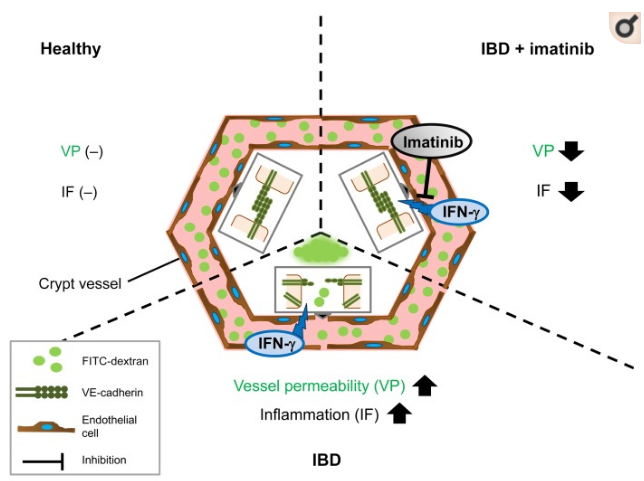
总之,该研究结果揭开了IFN-γ介导的肠道血管激活在IBD中的致病影响,并为该疾病的血管导向治疗开辟了新的途径。
原始出处:
Victoria Langer, Eugenia Vivi, et al., IFN-γ drives inflammatory bowel disease pathogenesis through VE-cadherin-directed vascular barrier disruption. J Clin Invest. 2019 Nov 1;129(11):4691-4707. doi: 10.1172/JCI124884.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#EST#
27
#IBD#
29
#IFN#
33
👍
67
了解
0
看来还是和肠道血管通透性有关!
0