Cardiovasc Diabetol:卡格列净对2型糖尿病合并慢性心衰患者NT-proBNP水平的影响
2021-09-17 Nebula MedSci原创
与格列美脲相比,卡格列净或可降低心室舒张功能较差的患者的 NT-pro BNP 水平
明确心力衰竭 (HF) 的有效治疗亚型是优化该疾病治疗的重要方向。Kusunose 等人推测 SGLT2 抑制剂 (SGLT2i) 对 N-末端脑钠肽前体 (NT-proBNP) 水平的有益影响可能取决于基线舒张功能。为了阐明 SGLT2i 在 2 型糖尿病 (T2DM) 和慢性 HF 中的作用,Kusunose 等人对 CANDLE 试验进行了一次事后亚研究,评估了卡格列净对 NT-proBNP 水平的影响,并根据基线左心室(LV)舒张功能进行分层。
CANDLE 试验的 233 位患者被随机分至添加卡格列净(n=113)或格列美脲治疗组(n=120)。主要终点是对比两组从基线到 24 周时 NT-pro BNP 水平的变化,并根据基线心室舒张功能进行分层。
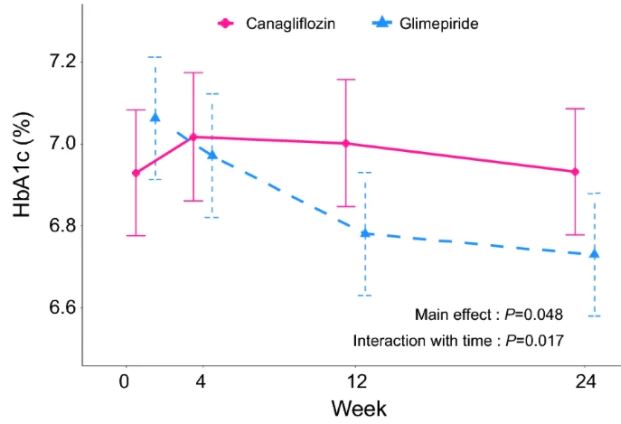
两治疗组的HbA1c水平变化
卡格列净组和格列美脲组从基线到 24 周时的 NT-pro BNP 的平均变化分别是 0.98(95% 0.89-1.08)和 1.07(95% CI 0.97-1.18)。卡格列净/格列美脲组的变化比是 0.93(95% CI 0.82-1.05)。应答者分析用于研究 NT-proBNP 水平改善的反应。
不同分组的NT-pro BNP水平变化
虽然室间隔环速度(SEP-e')的亚组分析显示,两治疗组间的效果没有明显的异质性;但 SEP-e'<4.7 cm/s 的亚组分析表明,与格列美脲组相比,卡格列净治疗与较低的 NT-proBNP 水平相关(卡格列净/格列美脲的变化比:0.83, 95% CI 0.66-1.04)。
综上,在 LV 舒张功能较低的亚组中,与格列美脲治疗相比,卡格列净组有 NT-pro BNP 水平降低的趋势。该研究表明,在根据 LV 舒张功能障碍严重程度分类的亚组中,卡格列净治疗的获益可能不尽相同。
原始出处:
Kusunose, K., Imai, T., Tanaka, A. et al. Effects of canagliflozin on NT-proBNP stratified by left ventricular diastolic function in patients with type 2 diabetes and chronic heart failure: a sub analysis of the CANDLE trial. Cardiovasc Diabetol 20, 186 (2021). https://doi.org/10.1186/s12933-021-01380-w
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#DIA#
37
#BET#
33
#ASC#
27
不错
61
#糖尿病#在 LV 舒张功能较低的亚组中,与格列美脲治疗相比,卡格列净组有 NT-pro BNP 水平降低的趋势
119
#BNP#
48
#NT-proBNP#
51
#心衰患者#
33
#PRO#
36
学习学习
48