JAMA Netw Open:主动或被动吸烟,均可导致儿童和青少年的血压升高!
2021-02-25 MedSci原创 MedSci原创
随着社会经济的发展和居民生活方式的改变,高血压已成为影响我国乃至全球居民健康的重大公共卫生问题之一。近40年来,以南非洲国家,南亚国家和一些太平洋岛国等中低收入国家高血压人数增幅最大,其中,2.26亿
随着社会经济的发展和居民生活方式的改变,高血压已成为影响我国乃至全球居民健康的重大公共卫生问题之一。近40年来,以南非洲国家,南亚国家和一些太平洋岛国等中低收入国家高血压人数增幅最大,其中,2.26亿高血压人口生活在中国。然而,46%的美国成年人饱受高血压之苦。虽然人们对成人高血压的认识、治疗和控制都在不断提高,但疗效仍不理想。
成人高血压临界值由心脑血管疾病和慢性肾脏疾病等在内的临床结果来定义,而小儿高血压则由统计学临界值来定义。虽然小儿高血压与心血管发病率和死亡率没有直接关系,但有大量证据显示小儿高血压与成人高血压相关。小儿高血压是生命健康中的一个重要因素,可能与成人慢病相关,包括心血管疾病、脑血管病和慢性肾脏病。因此,确定小儿高血压的可改变因素极为重要。

近日,发表在JAMA Netw Open杂志的一项显示,烟草暴露与儿童和青少年的血压升高(EBP)有关。在调整了潜在的混杂因素后,这种关联仍然存在。烟草暴露定义为血清可替宁水平大于0.05微克/升,或报告与吸烟者共同生活或自己吸烟。
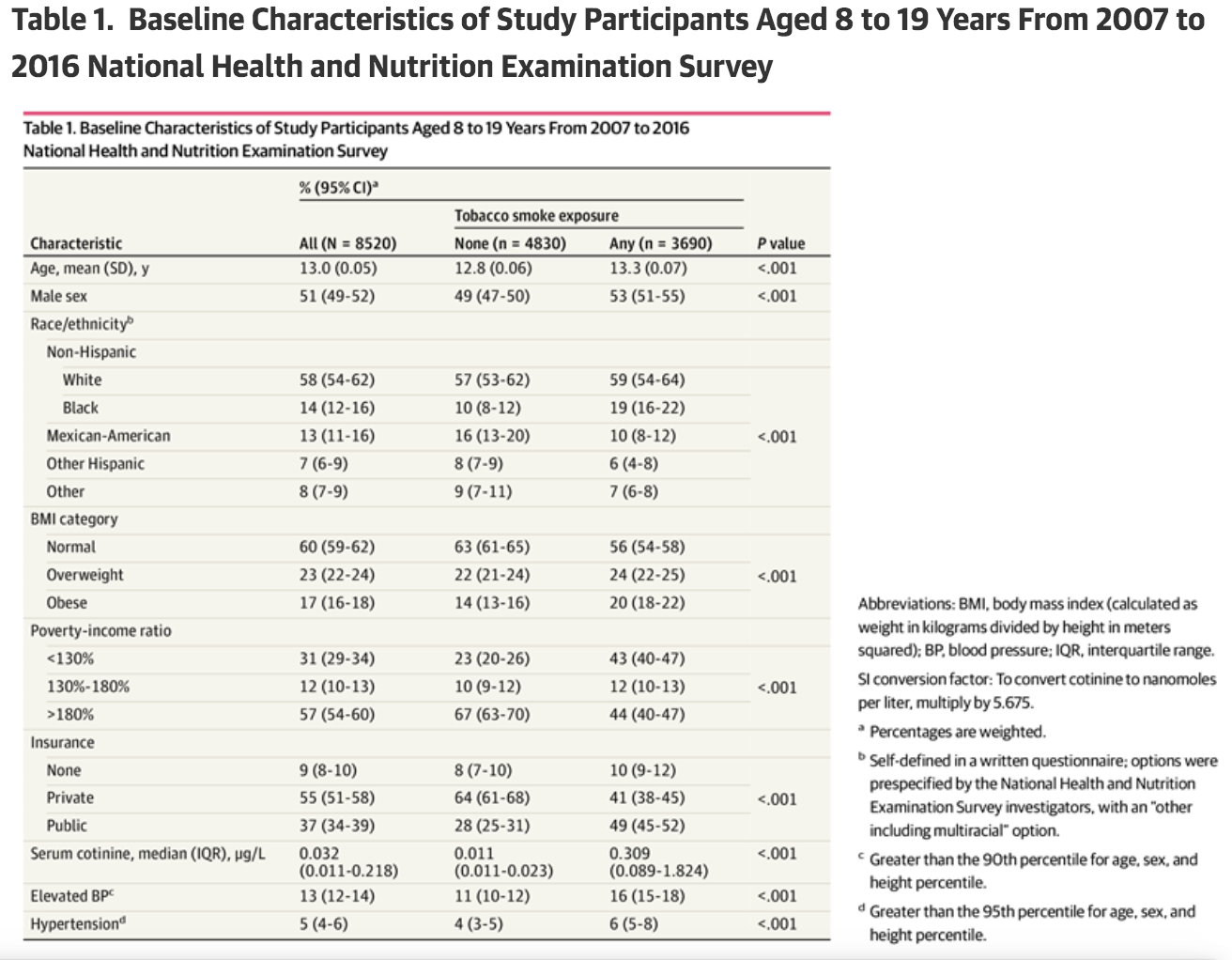
在这项横断面研究中,使用了2007年至2016年美国全国健康和营养检查调查(NHANES)的数据,这是一项基于人口的美国儿童和青少年全国代表性样本,共纳入8520名参与者,平均年龄为13.1岁,51%为男性。纳入标准主要是参与NHANES主研究时年龄为8至19岁,则符合条件。排除标准包括NHANES主研究的标准,无法完成测试,或缺少问卷。烟草暴露定义为血清可替宁水平大于0.05微克/升,或报告与吸烟者共同生活或自己吸烟。
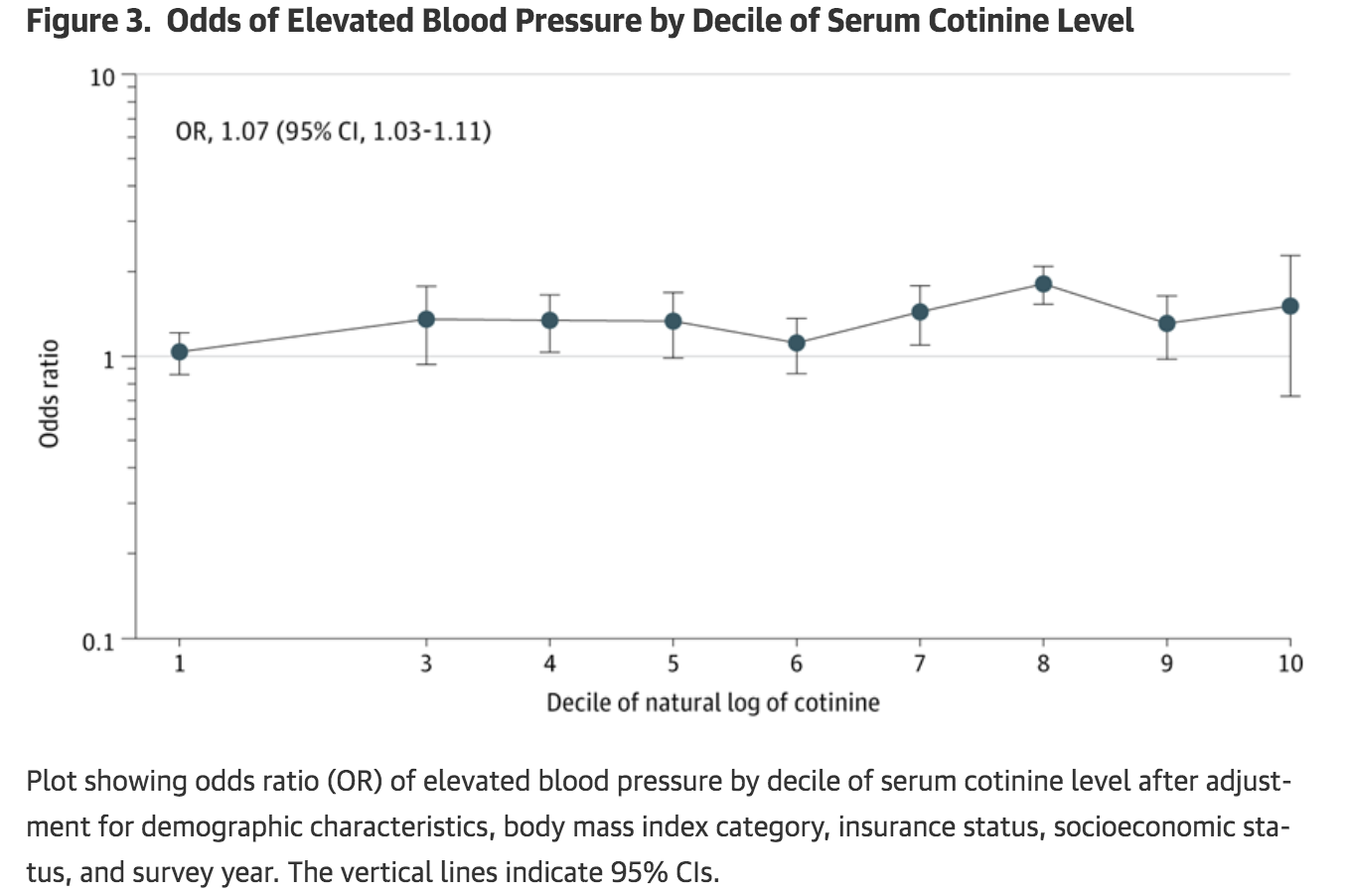
结果显示,在调整了人口统计学特征,体重指数,收入和保险状况之后,烟草暴露与EBP之间存在统计学上的显着关联。使用2种不同的异常血压定义来保持关联。不同年龄,性别和种族/族裔定义的不同参与者亚组之间的关联性相似。最后,使用不同吸烟状态定义的敏感性分析显示出可比的关联性。
因此,儿童接触烟草与EBP的关联具有重要的公共卫生意义,将购买烟草制品的法定年龄提高到21岁,将使2010年至2019年期间出生的美国人减少24.9万人的过早死亡,减少420万生命年的损失。由于儿童时期的血压与成年后的血压相关,而成人高血压是心血管疾病的危险因素,因此儿童EBP的可改变的危险因素是公共卫生运动的潜在目标。
原始出处
Rebecca V. Levy, et al.Analysis of Active and Passive Tobacco Exposures and Blood Pressure in US Children and Adolescents.JAMA Netw Open. 2021;4(2):e2037936. doi:10.1001/jamanetworkopen.2020.37936
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#血压升高#
37
#NET#
31
#儿童和青少年#
42
!
64
#PE#
29
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
57