Nature Genet:测序发现肺腺癌脑转移的驱动因素
2020-03-27 小通 生物通
为了鉴定促进脑转移的基因组改变,美国Dana-Farber癌症研究所、Broad研究所等机构的研究人员对73例肺腺癌脑转移病例进行全外显子组测序。他们追踪到一些复发性驱动基因突变,与肺腺癌的脑转移一致
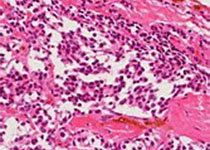
肺腺癌(lung adenocarcinoma)是肺癌的一种,属于非小细胞癌。不同于鳞状细胞肺癌,它较容易发生于女性及不抽烟者。大约一半的肺腺癌患者会发生脑转移,这使得治疗更加棘手。
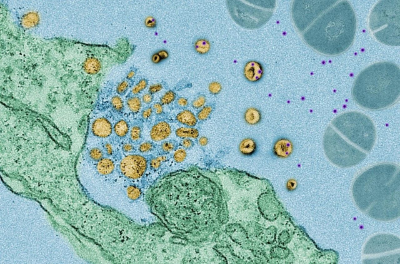
为了鉴定促进脑转移的基因组改变,美国Dana-Farber癌症研究所、Broad研究所等机构的研究人员对73例肺腺癌脑转移病例进行全外显子组测序。他们追踪到一些复发性驱动基因突变,与肺腺癌的脑转移一致。这些成果于3月23日发表在《Nature Genetics》杂志上。
作者在文中写道:“这些结果表明,体细胞改变促进了脑转移,而且足够数量的转移性肿瘤的基因组测序可以揭示出以往未知的转移驱动因素。”
研究人员对肺腺癌患者的脑转移样本的外显子组进行测序,并将这些数据与500多个原发性肺腺癌的外显子组进行比较。他们发现,少数拷贝数变化在脑转移瘤中较为常见,包括MYC、YAP1和MMP13扩增以及CDKN2A / B缺失。
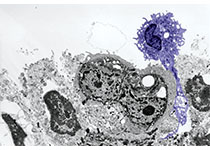
研究团队接着利用另外105个转移性脑肿瘤样本以及MYC、YAP1和MMP13水平高于正常水平的小鼠异种移植肿瘤模型,通过荧光原位杂交(FISH)验证了这些结果。
“我们鉴定出的候选驱动因素代表了脑转移的潜在治疗靶点,”作者写道,并指出“带有YAP1扩增的脑转移可能是Hippo通路抑制剂的潜在目标,这种抑制剂正在积极开发中。”
当然,肺腺癌的脑转移是一个复杂的过程。研究人员表示:“尽管我们已经确定了体细胞的遗传改变会驱动原发性肿瘤形成,但尚不清楚其他遗传改变是否也促进了脑转移的发展。”
在这项研究中,研究人员对73例肺腺癌患者的脑转移样本中的外显子部分进行测序,并将其结果与503个原发性肺腺癌肿瘤样本的序列进行比较。他们注意到,与原发性肿瘤相比,脑转移的特点是扩增明显增加,包括含有MYC、YAP1和MMP13基因的基因组区域。同时,CDKN2A/B区域往往发生缺失。
研究人员随后对另外105个转移性肿瘤样本开展FISH分析,以确认之前发现的结果。他们发现了相同的扩增和缺失。例如,98个样本中的9个含有YAP1和MMP13的扩增。而MYC扩增则更为常见,在94个样本中的20个出现。
之后,他们使用了过表达MYC、YAP1和MMP13的小鼠异种移植肿瘤模型,发现实验结果支持了这些基因的扩增可能增加肺部肿瘤向大脑转移的可能性。不过,他们指出,驱动转移的DNA改变可能并不是脑转移瘤形成所必需的。
原始出处:Shih DJH, Nayyar N, Bihun I, et al. Genomic characterization of human brain metastases identifies drivers of metastatic lung adenocarcinoma. Nat Genet. 2020 Mar 23.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Nat#
32
#Genet#
24
#NET#
28
#Gene#
21
#驱动因素#
34