JCO:rCOJEC,国际高危神经母细胞瘤患者的**诱导方案
2021-06-22 Nebula MedSci原创
rCOJEC方案是国际儿科肿瘤学会欧洲神经母细胞瘤组的首选诱导方案
诱导治疗是高危神经母细胞瘤治疗的重要组成部分。本研究旨在评估纪念斯隆凯特琳癌症中心(MSKCC)N5诱导方案(MSKCC-N5),与快速COJEC(rCOJEC:顺铂[C]、长春新碱[O]、卡铂[J]、依托泊苷[E]和环磷酰胺[C])相比,是否可改善高危神经母细胞瘤患者的转移完全缓解(mCR)率和3年无事件生存率(EFS)。
招募了1-20岁的4期神经母细胞瘤患者或1岁以内的携带MYCN扩增的4/4s期患者,随机分至rCOJEC组或MSKCC-N5组。诱导化疗后,予以包括原发肿瘤切除、大剂量白消安和美法仑、原发肿瘤部位放疗、异维A酸与ch14.18/CHO抗体联合或不联合白介素-2免疫疗法在内的系统治疗。主要终点是mCR率和3年EFS。
共630位患者被随机分至rCOJEC组(n=313)或MSKCC-N5组(n=317)。确诊时的中位年龄为3.2岁(范围1个月-20岁),16位携带MYCN扩增的不足一岁的患儿。
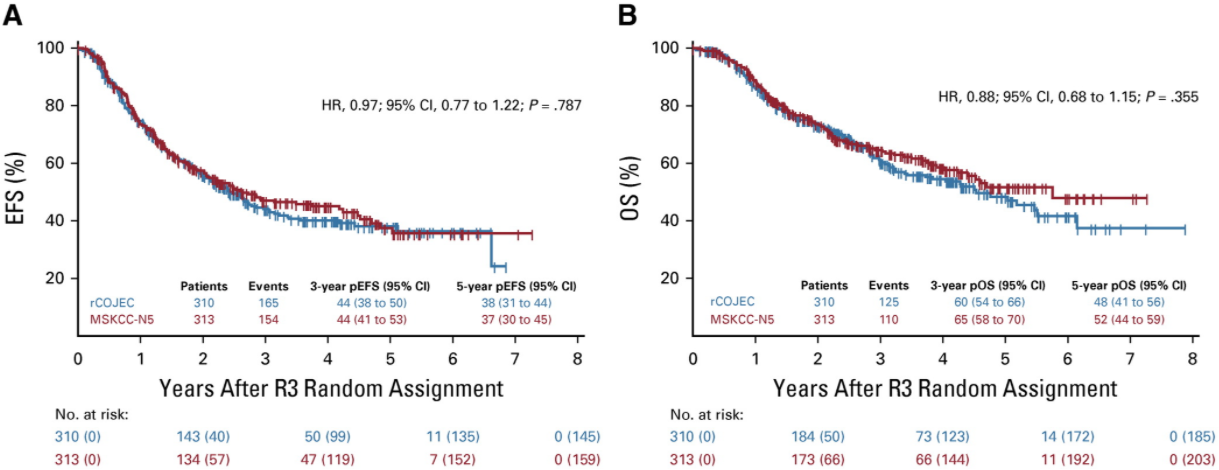
两组患者的EFS和OS
rCOJEC诱导化疗后的mCR率(32%)与MSKCC-N5后的无明显差异(35%;p=0.368),3年EFS分别是44%±3%(rCOJEC)和47%±3%(MSKCC-N5;p=0.527)。rCOJEC组和MSKCC-N5组的3年总存活率分别是60%±3%和65%±3%(p=0.379)。
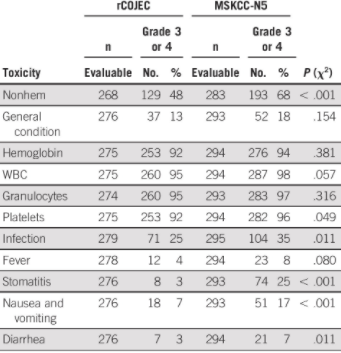
两组的部分3/4级毒性反应
两种治疗方案的毒性死亡率均为1%。但是,MSKCC-N5诱导化疗的非血液学 CTC 3/4级毒性事件发生率更高(68% vs 48%;p<0.001):感染(35% vs 25%;p=0.011)、口炎(25% vs 3%;p<0.001)、恶心和呕吐(17% vs 7%;p<0.001)和腹泻(7% vs 3%;p=0.011)。
综上所述,rCOJEC和MSKCC-N5两种诱导方案的疗效预后未见明显差异;但rCOJEC方案的急性毒性事件更少,因此,rCOJEC方案是国际儿科肿瘤学会欧洲神经母细胞瘤组的首选诱导方案。
原始出处:
Alberto Garaventa, et al. Randomized Trial of Two Induction Therapy Regimens for High-Risk Neuroblastoma: HR-NBL1.5 International Society of Pediatric Oncology European Neuroblastoma Group Study. Journal of Clinical Oncology. June 21, 2021. https://ascopubs.org/doi/full/10.1200/JCO.20.03144
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#JCO#
36
#母细胞瘤#
33
#细胞瘤#
27
实用
45