Front Oncol:非转移性非透明细胞肾细胞癌(non-ccRCC)患者的临床特征和临床预后差异
2022-01-11 yd2015 MedSci原创
研究表明,与其他RCC亚型相比,集合管和肉瘤样组织学亚型并不常见,且与术后较差的生存率相关。需要进一步的研究来评估新辅助和辅助全身治疗在这些亚型中的作用。
非透明细胞肾细胞癌(non-ccRCC)包括组织学和分子上不同的亚型,如乳头状、嫌色、集合管和肉瘤样RCC,发病率为20% - 25%。非透明细胞肾细胞癌的肿瘤预后和辅助全身治疗(血管内皮生长因子抑制因子(VEGFi)或免疫治疗)的作用尚不明确。因此,美国学者开展了回顾性研究,评估non-ccRCC亚型与ccRCC亚型的发病率和生存结局。相关结果发表在Frontiers in Oncology杂志上。
研究利用国家癌症数据库在2004年至2015年间筛查非转移性RCC (T1-4, N0-1)患者。Non-ccRcc队列进一步按组织学亚型分层:乳头状、嫌色性、肉瘤样和集合管型RCC。采用多变量Cox回归模型比较总生存期(OS)。
总的来说,我们的分析纳入了220,170例RCC患者。共有178,066名患者为非转移性ccRCC, 42,104名患者为non-ccRCC。大多数non-ccRCC队列由乳头状和嫌色亚型组成,分别有27510(65.3%)和12760(30.3%)例。
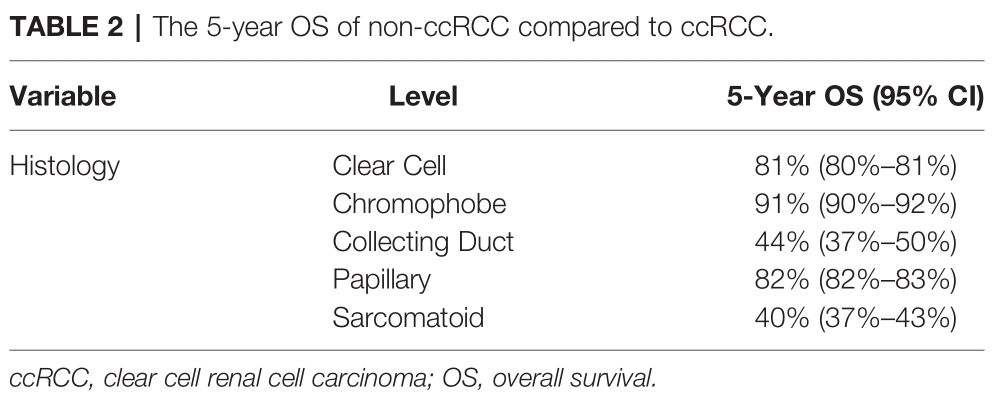
所有组织学亚型患者的中位随访时间为48.5个月。嫌色性RCC与良好的OS相关,5年OS为91%。透明细胞亚型和乳头状亚型的5年OS分别为82%和81%。集合管型和肉瘤样RCCs的预后较差,5年OS分别为44%和40%。
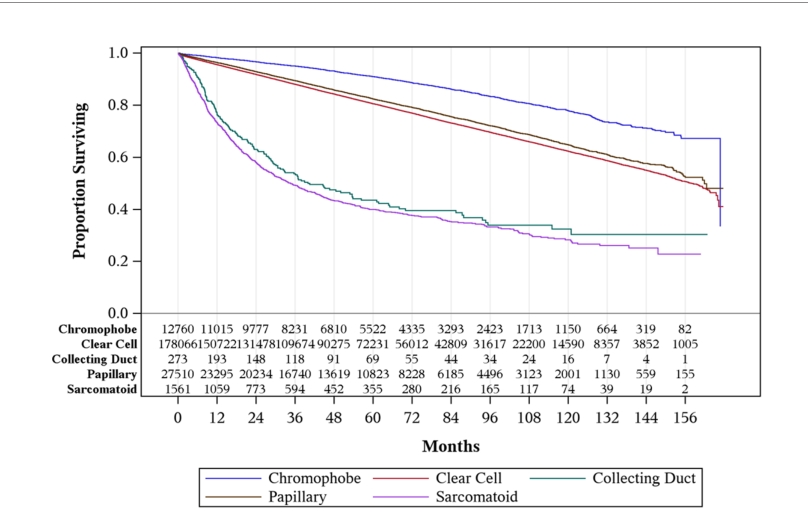
非透明细胞肾细胞癌(non-ccRCC)各亚型预后差异
多变量分析包括6723例嫌色、188例集合管、19086例乳头状和1083例肉瘤样RCC。与<65岁患者相比,≥65岁患者的生存率较差(HR = 1.75, 95% CI: 1.69-1.82)。与女性相比,男性预后较差(HR = 1.16, 95% CI: 1.13 1.19)。与白人相比,黑人的OS较短(HR = 1.11, 95% CI: 1.06 1.16),而西班牙裔(HR = 0.76, 95% CI 0.72 0.81)和其他族裔(HR = 0.82, 95% CI 0.75 0.90)的生存率较高。
高分化(HR = 0.71, 95% CI: 0.69-0.73)和中分化(HR = 0.70, 95% CI: 0.67-0.73)患者的预后较好。与I期患者相比,II期(HR = 1.35, 95% CI: 1.31-1.40)和III期(HR = 1.94, 95% CI: 1.88-2.00)预后较差。

亚组分析
在手术治疗方面,与根治性切除相比,无手术治疗(HR = 2.92, 95% CI: 2.68 3.18)和消融/切除(HR = 1.19, 95% CI: 1.12 1.27)预后较差。有趣的是,与根治性切除相比,部分切除可改善OS (HR = 0.61, 95% CI: 0.58 0.63),而单纯切除与根治性切除的OS无明显差异。
与无区域淋巴结手术相比,区域淋巴结手术与较差的生存结局相关(HR = 1.24, 95% CI: 1.19-1.28)。放射治疗(HR = 1.90, 95% CI: 1.58 2.29)与不良结局相关,接受化疗的患者的生存期较差(HR = 1.79, 95% CI: 1.64 1.95)。相对于透明细胞亚型,集合管(HR = 2.26, 95% CI: 1.82—2.82)和肉瘤样(HR = 2.60, 95% CI: 2.33—2.91)患者预后较差,嫌色细胞亚型(HR = 0.64, 95% CI: 0.59—0.68)预后较好,而乳头状亚型(HR = 1.03, 95% CI: 0.99—1.07)没没有明显差异。
综上,研究表明,与其他RCC亚型相比,集合管和肉瘤样组织学亚型并不常见,且与术后较差的生存率相关。需要进一步的研究来评估新辅助和辅助全身治疗在这些亚型中的作用。
原始出处:
An J, Packiam VT, Chennamadhavuni A, Richards J, Jain J, Mott SL and Garje R (2022) Patient Characteristics and Survival Outcomes of Non-Metastatic, Non-Clear Cell Renal Cell Carcinoma. Front. Oncol. 11:786307. doi: 10.3389/fonc.2021.786307
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#非转移#
35
#RCC#
34
#临床特征#
30
#CRC#
41
#细胞癌#
34
#Oncol#
23
#非转移性#
32
#预后差异#
33
#转移性#
27
#临床预后#
45