HBP:机器学习使用高阶功能连接可以区伴有或不伴有认知障碍的2型糖尿病与健康人群
2021-07-19 MedSci原创 MedSci原创
跨大规模脑内网络的dFC存在鉴别同步性,可以将T2DM-CI(和T2DM-noCI)与HC区分开来。
2型糖尿病(T2DM)与认知障碍相关,并可能进展为痴呆。然而,对T2DM相关性痴呆的脑功能机制仍知之甚少。近年来的静息状态功能性磁共振成像功能连接性(FC)研究证明了其在T2DM合并认知功能损害(T2DM-CI)研究中的潜在价值。然而,由于敏感性较低,他们主要采用单因素统计分析,不适于揭示T2DM-CI中FC“模式”的改变。
近期,Human Brain Mapping 杂志发表文章提出利用高阶FC来揭示T2DM-CI中的异常连接模式,并采用多元的、基于机器学习的策略。
为了更好地了解T2DM引起的认知功能损害,该研究对23例T2DM-CI和27例T2DM-noCI患者以及50例健康对照(HCs)进行了研究,研究了T2DM-CI和T2DM无认知功能损害(T2DM-noCI)之间的这种模式是否不同。首先基于多个脑区对之间的动态FC时间序列的时间同步建立大规模高阶脑网络,然后利用这些信息从匹配的HC中基于支持向量机分类T2DM-CI(以及T2DM-noCI)。
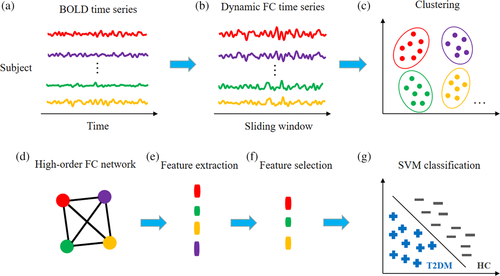
基于动力学的高阶功能连接(dHOFC)网络构建框架及2型糖尿病伴认知功能障碍(T2DM-CI)与健康对照组(HC)的网络分类。
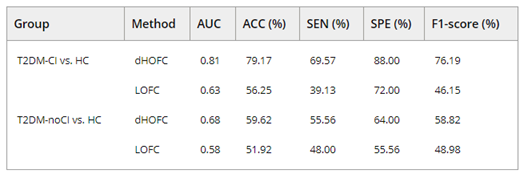
T2DM-CI与HC以及T2DM-noCI与HC的区分表现
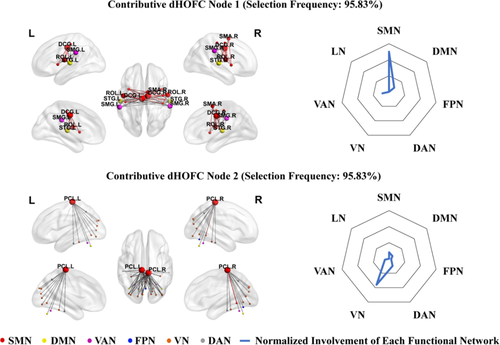
左面板显示了根据选择频率(95.83%)从2型糖尿病伴认知功能障碍(T2DM-CI)和健康对照(HC)之间的分类中选择的前两个基于区分动力学的高阶功能连接(dHOFC)节点。

基于动力学的高阶功能连接性(dHOFC)特征的散点图[(a)和(b)分别表示dHOFC节点1和节点2的局部聚类系数,与2型糖尿病合并认知损害(T2DM-CI)组蒙特利尔认知评估(MoCA)得分相比较。
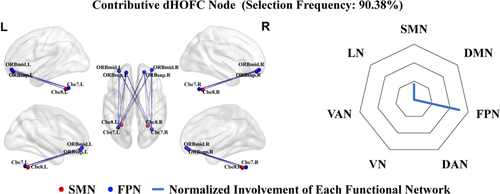
左面板显示从无认知障碍的2型糖尿病(T2DM-noCI)和健康对照(HC)的分类中,根据选择频率(90.38%)选择的第1个区分性动态高阶功能连接(dHOFC)节点。
该研究模型在T2DM-CI与HC的鉴别诊断中获得了79.17%的准确率,但在T2DM-noCI与HC的分类诊断中仅获得了59.62%的准确率。T2DM-CI与HC相比存在异常的高阶FC模式,这与T2DM-NOCI不同。
该研究是首次基于脑功能网络对T2DM-CI和HC以及T2DM-noCI和HC进行分类研究。使用脑dHOFC网络来提高检测疾病引起的脑功能变化的灵敏度。结果表明,跨大规模脑内网络的dFC存在鉴别同步性,可以将T2DM-CI(和T2DM-noCI)与HC区分开来。通过构建dHOFC网络,并借助机器学习进行基于网络的分类,首次揭示了与T2DM所致认知损害相关的几种共变异dFC,其中一些dFC与MoCA和AVLT-IR评估的患者认知能力显著相关。基于dHOFC的T2DM-noCI与HC的分类不如T2DM-CI与HC的分类,且dHOFC特征不同,提示T2DM-CI涉及严重的脑功能障碍,可能不同于T2DM-noCI。该研究提供了有价值的信息,可能有助于理解T2DM相关的中枢神经系统的改变。
该研究表明,T2DM引起的认知功能损害可能存在广泛的功能连接改变。这一结果有助于更好地理解T2DM引起的中枢神经系统的变化。
原文出处
Classification of type 2 diabetes mellitus with or without cognitive impairment from healthy controls using high-order functional connectivity. https://doi.org/10.1002/hbm.25575
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#健康人#
53
#功能连接#
42
#机器#
35
谢谢MedSci提供最新的资讯
0
学习了
82
加油
0