J Immunother Cancer:PD-1抑制剂联合化疗新辅助治疗可切除食管鳞状细胞癌患者的疗效
2022-01-14 yd2015 MedSci原创
研究表明,卡瑞利珠单抗联合白蛋白结合型紫杉醇+卡铂新辅助治疗可切除ESCC患者疗效显著且安全可控。
PD-1抑制剂新辅助治疗可切除食管鳞状细胞癌(ESCC)患者的疗效尚不明确。因此,来自中山大学附属第一医院团队开展相关研究,评估PD-1抑制剂联合化疗新辅助治疗可切除食管鳞状细胞癌患者的疗效。相关结果发表在J Immunother Cancer杂志上。
研究纳入既往未治疗、可切除的(II或III期)ESCC患者。患者接受了2疗程的卡瑞利珠单抗、白蛋白结合型紫杉醇和卡铂的新辅助治疗,在第一个周期后约6 - 9周进行手术切除。
2020年1月至2020年9月期间,筛查了37名患者,其中23人入组。入组患者年龄58.6±10.1岁。队列中的大多数(69.6%)是吸烟者,大多数患者(95.7%)是男性。肿瘤位于食管下段13例(56.5%),食管中段9例(39.1%),食管上段1例(4.3%)。
20例患者进行手术,所有患者均进行了R0切除,并没有观察到手术延迟。5例(25%)患者有病理完全缓解(PCR), 10例(50%)患者有主要病理缓解(MPR)。ORR和DCR分别为90.5%(19 / 21)和100%(21 / 21)。16例(80%)患者达到临床T期病理降期;10例(50%)患者达到临床N期的病理降期;13例(65%)患者达到了临床总分期的病理下分期。
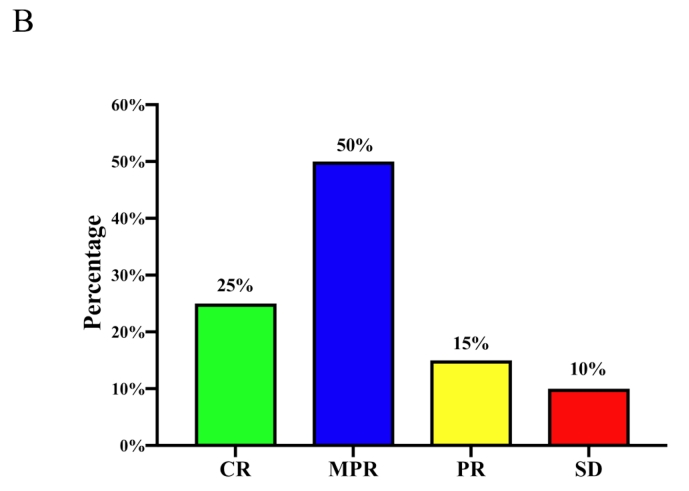
疗效评估
在23例患者中,脱发是最常见的治疗相关AE,发生率为82.6%。乏力(65.2%)、中性粒细胞减少(60.9%)、白细胞减少(60.9%)、皮疹(60.9%)、贫血(56.5%)和谷丙转氨酶升高(43.5%)也是常见不良反应。
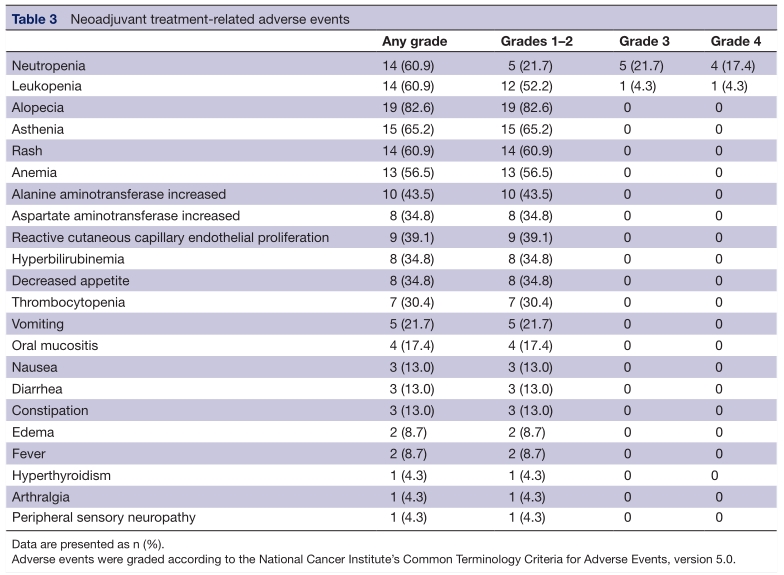
不良反应
在接受手术的整个队列患者中,中位无病生存期(DFS)未达到。与获得PCR的患者,未获得PCR患者的DFS没有显著差异。在10例MPR患者中,病理分期为T2/T3的患者肿瘤复发或转移的风险高于T1/Tis患者(p=0.033)。
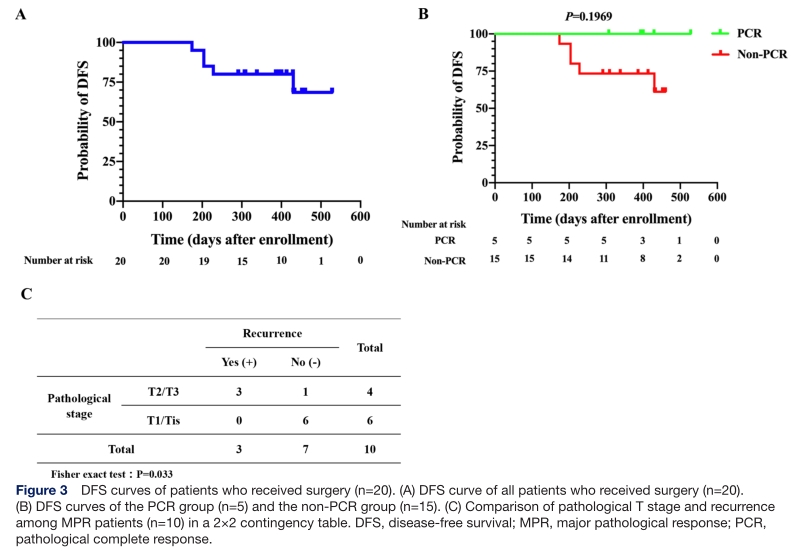
预后分析
在原发肿瘤中,高突变负荷和高表达程序性死亡配体1 (PD- L1)的患者比例在PCR组中显著高于非PCR组(p=0.044)。治疗后,PCR组PD- L1 + CD163 +浸润细胞数明显低于非PCR组(p=0.017)。
综上,研究表明,卡瑞利珠单抗联合白蛋白结合型紫杉醇+卡铂新辅助治疗可切除ESCC患者疗效显著且安全可控。
原始出处:
Yang W, Xing X, Yeung SJ, Wang S, Chen W, Bao Y, Wang F, Feng S, Peng F, Wang X, Chen S, He M, Zhang N, Wang H, Zeng B, Liu Z, Kidane B, Seder CW, Koyanagi K, Shargall Y, Luo H, Peng S, Cheng C. Neoadjuvant programmed cell death 1 blockade combined with chemotherapy for resectable esophageal squamous cell carcinoma. J Immunother Cancer. 2022 Jan;10(1):e003497. doi: 10.1136/jitc-2021-003497. PMID: 35022193.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#细胞癌#
34
#抑制剂#
28
#新辅助#
30
#PD-1抑制剂#
34
#食管鳞状细胞癌#
54
#联合化疗#
40
#食管#
28
学习学习了
42