荷兰肺动脉高压队列中性激素和长期右心室适应的相互作用
2022-01-24 刘少飞 MedSci原创
肺动脉高压(PAH)是一种以肺小动脉狭窄和右心衰竭为特征的进行性疾病。本研究荷兰不同年龄的肺动脉高压 (PAH) 患者队列中性激素表达改变与长期右心室 (RV) 适应和右心衰竭进展之间的关联。
性别差异在心血管生理和疾病中很常见。对4000 名健康社区参与者进行的动脉粥样硬化(MESA)多种族研究表明,与年龄匹配的男性相比,女性的 RV 质量和体积较小,而RV 射血分数(RVEF) 较高。在很大程度上,这种区别可以用性激素水平的差异来解释,尤其是雌激素。在使用激素替代疗法 (HRT)的健康绝经后妇女中,较高的 RVEF 和较低的 RV 收缩末期容积与较高的雌激素血清水平相关。肺动脉高压(PAH)是一种以肺小动脉狭窄和右心衰竭为特征的进行性疾病。虽然女性更容易发生 PAH(女性:男性患病率 ∼2:1),但她们的生存率明显优于男性患者。先前的研究表明,女性的这种生存益处可能是由不同的 RV 对治疗的反应来解释的。
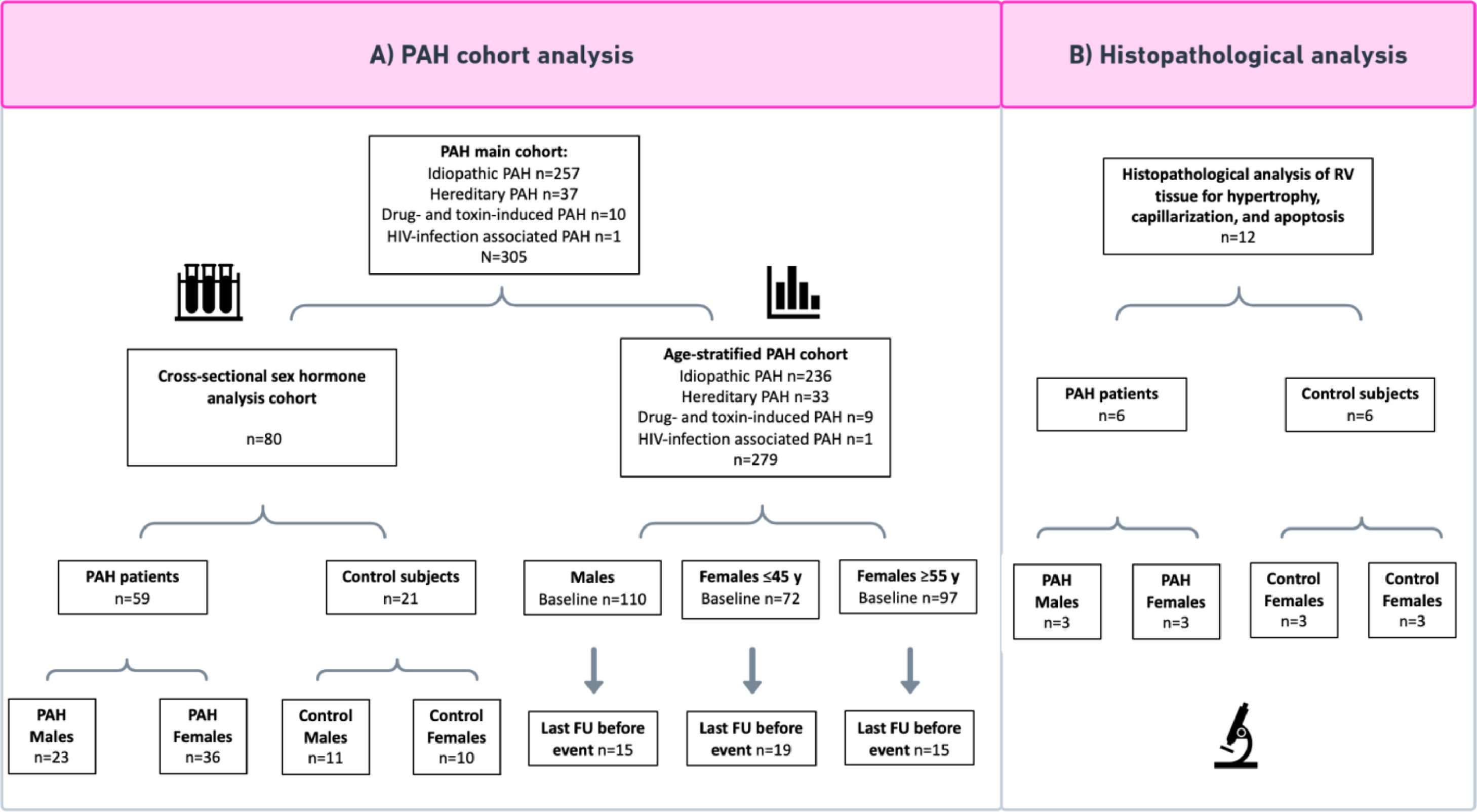
在 PAH 中也观察到不同的性激素表达水平。特别是高雌二醇和减少的脱氢表雄酮硫酸盐 (DHEA-S) 与男性和绝经后女性的 PAH 严重程度有关。此外,几项动物研究调查了性激素对肺血管重塑和RV 衰竭的影响。然而,由于患者和动物模型之间的数据相互矛盾,并且由于育龄年轻女性的数据有限,性激素与 RV 适应之间的确切关联仍然难以捉摸。此外,大多数关于性激素的数据都是在美国中心获得的。由于已知美国和欧洲患者在人口统计学特征和 HRT 使用方面存在差异,因此在非美国 PAH 队列中研究性激素也很重要。最后,大部分数据是横断面数据或病程中某一时间点的数据,而RV 功能的纵向数据在向右心衰竭发展的过程中,对于了解男性和女性患者之间不同的 RV 适应模式至关重要。因此,在本研究中,我们旨在调查性激素表达水平改变与 RV 适应之间的关联,并评估荷兰不同年龄患者队列中右心衰竭随时间的进展情况。我们进行了一项转化研究,其中我们将性激素的横断面分析与 RV 适应的纵向分析和来自女性和男性 PAH 患者的 RV 组织的组织病理学分析相结合。
研究方法:
在这项研究中,我们纳入了 279 名 PAH 患者,其中 169 名女性和 110 名男性。我们从 59 名患者和 21 名对照中收集血浆样本进行性激素分析。在基线时进行右心导管(RHC) 和/或心脏磁共振 (CMR) 成像。对于纵向数据分析,我们选择了在事件发生前最多 1.5 年接受 RHC 和/或 CMR 的患者(死亡或移植,N = 49)。
研究结果:
PAH 引起的生存、右室功能和适应的性别差异。
我们纳入了 236 名特发性 PAH、33 名可遗传 PAH、9 名药物和毒素诱导的 PAH 以及 1 名与 HIV 感染相关的 PAH 患者,在年龄分层的 PAH 队列中总共有 110 名男性和 169 名女性患者(N = 279 )。
与对照组相比,男性和女性 PAH 患者的脱氢表雄酮硫酸盐 (DHEA-S) 水平降低,而雄烯二酮和睾酮仅在女性患者中降低。
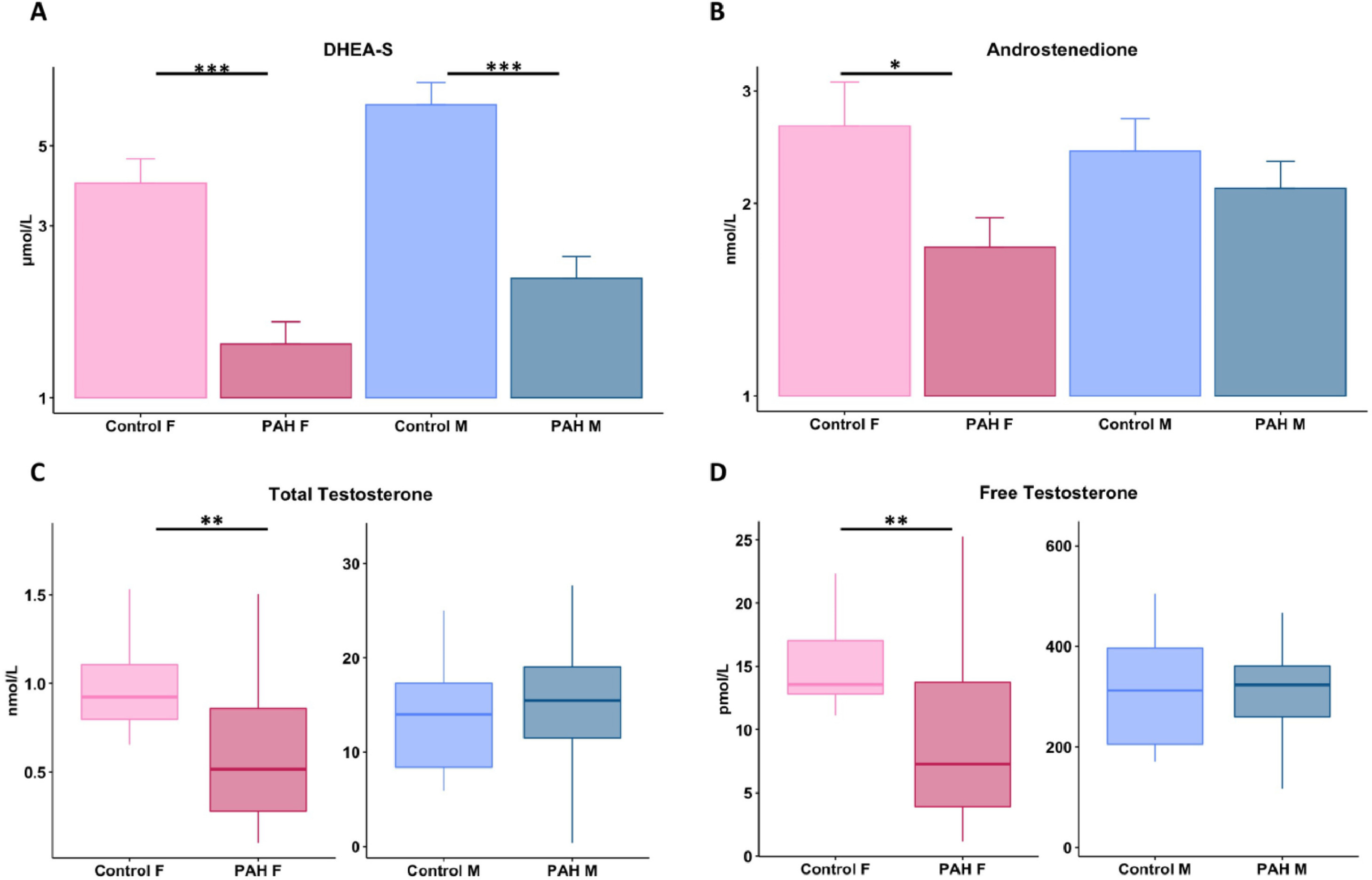
有趣的是,低 DHEA-S 和高睾酮水平仅与男性患者较差的RV 功能相关。随后,我们分析了按年龄分层的女性的预后和 RV 适应。与≥55岁的女性和男性相比,≤45岁的女性预后最好。
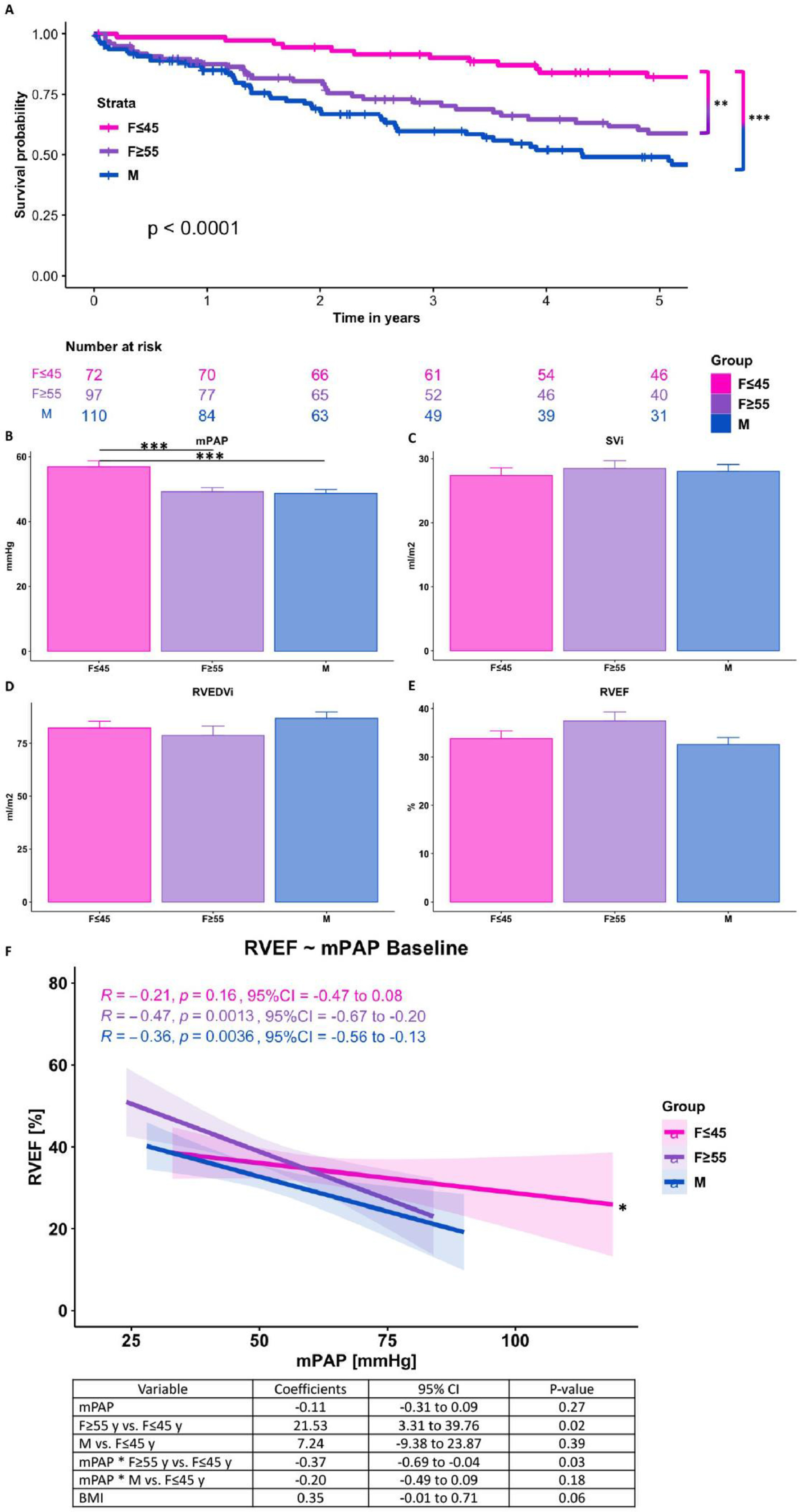
尽管 ≤45 岁的女性压力超负荷较高,但在基线时未观察到 RV 功能差异。纵向数据表明 RV 适应有明显区别。尽管 ≤45 岁的女性在较晚的时间点发生了事件,但 RV 功能在终末期疾病时受损程度更大。
研究启示:
在男性和女性 PAH 患者中,性激素与 RV 功能的相关性不同。男性和女性 PAH 患者的 DHEA-S 似乎较低。≤45 岁的女性可以更长时间地承受压力超负荷,但在疾病终末期有更严重的 RV 表型。
文献参考:
van Wezenbeek J. Interplay of sex hormones and long-term right ventricular adaptation in a Dutch PAH-cohort. J Heart Lung Transplant. 2021 Nov 14:S1053-2498(21)02581-X. doi: 10.1016/j.healun.2021.11.004. Epub ahead of print. PMID: 35039146.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#相互作用#
56
#动脉高压#
33
#性激素#
49
#互作#
49
#右心室#
41