EClinicalMedicine:国药新冠疫苗接种第3剂,中和抗体能达到什么水平?
2021-07-27 MedSci原创 MedSci原创
新冠病毒突变,大量已接种新冠疫苗人群出现了“突破性感染”,此次南京疫情,感染者大部分都已接种过两剂新冠疫苗,这不禁让人疑问:疫苗的保护作用如何?当然,新冠疫苗接种以后,随着时间
新冠病毒突变,大量已接种新冠疫苗人群出现了“突破性感染”,此次南京疫情,感染者大部分都已接种过两剂新冠疫苗,这不禁让人疑问:疫苗的保护作用如何?当然,新冠疫苗接种以后,随着时间推移,体内中和抗体水平会明显下降,从而降低对病毒的防护作用。
目前有超过24种SARS-CoV-2疫苗(7个蛋白亚单位、6个灭活、6个重组、3个mRNA、1个DNA、1个病毒样颗粒疫苗)不同阶段临床试验结果。对于国药控股(中国武汉)开发的灭活疫苗,我们之前已经报道了 18-59 岁成年人的三剂量组 1 期试验和 0 天和 14/21 天组的 2 期试验中期结果。6·0%~25·0%的参与者出现不良反应,全程接种后第14天中和抗体滴度在121~316之间。
目前国际上普遍认为需要第三针新冠疫苗。刚刚科兴灭活疫苗发表了3针的结果,即在两剂接种后第6个月再接种1剂(即第3剂),体内中和抗体的滴度水平会上升。结果表明,接种第三剂后能够迅速诱导强烈的免疫反应,中和抗体滴度显著提高,接种第三剂后28天中和抗体滴度比第二剂后28天中和抗体滴度增加了3-5倍,详细见:科兴生物发布重磅研究结果!接种第三剂科兴新冠灭活疫苗后中和抗体水平显著增高
在国际上,辉瑞mRNA新冠疫苗也在部分人群中开始接种第3针,在国内随着mRNA临近获批,有些人认为可以把mRNA疫苗作为第3针加强针使用。同时,不同疫苗的混接也较为普遍,最典型的是加拿大,最先混接的国家。有研究表明,如果第一针是腺病毒疫苗,然后再接种mRNA疫苗,可能会诱导强烈的免疫反应,中和抗体滴度大幅度上升。
在国内,普遍接种的是国药灭活新冠疫苗,那么,国药的疫苗接种第3针会是什么样的结果呢?梅斯医学小编告诉你答案!
刚刚发表一项 1/2 期、随机、双盲、安慰剂对照试验,由武汉生物制品研究所有限公司和河南省疾病预防控制中心(CDC)设计,研究方案获得批准。研究人员自 2020 年 4 月 12 日起进行了正在进行的试验并收集了数据。独立的数据和安全监测委员会 (DSMB) 在试验期间监测了安全数据并评估了参与者的风险。试验在www.chictr.org.cn(ChiCTR2000031809)注册,受试者年龄≥6岁;然而,只有在评估了成人接种后 28 天的安全性和免疫原性结果后,才开始对儿童和青少年进行干预。因此,针对儿童和青少年的试验仍在进行中,尚无数据可用。目前的分析仅包括 18 岁及以上的成年人。
在 1 期试验中,受试者按 18-59 岁(年轻人)和 60 岁以上(老年人)进行分层,随机分配以接受 2.5 微克、5 微克或 10 微克的灭活 SARS-CoV-2 疫苗或安慰剂,在第 0、28 和 56 天通过肌肉注射(每组 24 名参与者)。为加快疫苗研发并为3期试验提供相关数据,2期试验与1期试验同时设计,采用相同的分组方法(即疫苗2.5微克、5微克、在年轻人和老年人中,分别在第 0、28 和 56 天使用 10 μg 和 10 μg 安慰剂,每组样本量更大(每组 60 名参与者)。为了快速提高人群中的疫苗覆盖率,在 2 期试验中又增加了 4 个年龄在 18-59 岁之间的组,以探索更少的剂量或更短的剂量间隔是否也可能具有免疫原性,即两第 0 天和第 14 天、第 0 天和第 21 天或第 0 天和第 28 天的 5 μg 剂量计划,或第 0 天的 10 μg 单剂量计划(疫苗:安慰剂 = 每组 3:1)。
受试者依次入组并以年龄和剂量递增的方式接受注射。第 1 期试验的第一组 18-59 岁参与者首先接受 2.5 μg 的灭活疫苗,并在第一次注射后监测不良事件 7 天。如果没有观察到严重的不良事件,1 期试验中 18-59 岁的第二组参与者接受了 5 μg 的灭活疫苗;同时,1 期试验中年龄≥60 岁的一组参与者和 2 期试验中 18-59 岁的参与者接受了 2.5 μg 的灭活疫苗。类似的序列用于 5 μg 和 10 μg 组(补充附录,图 1)。参与者、研究人员和实验室人员对干预分配不知情。
主要的体液免疫原性结果是在全程接种后第 28 天和第 90 天测量的中和抗体滴度和特异性 IgG 结合抗体滴度。将 1 期和 2 期试验中同一时间点的抗体滴度合并在一起分析。在第一阶段试验中,还在每次给药前、每次注射后第 4 天以及第一次和第二次注射后的第 14 天收集血样,在这些时间点测量的中和抗体滴度和特异性 IgG 结合抗体滴度是次要的免疫原性结果。
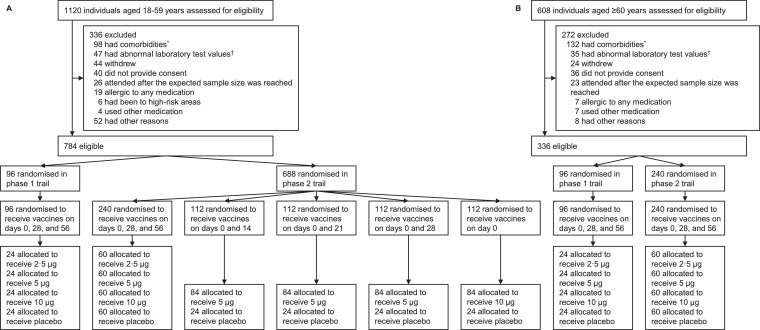
Screening, randomization, and inclusion in safety and immunogenicity analyses stratified by age groups
结果表明,全程接种后第 90 天中和抗体滴度的 GMT 为 87(95% CI,61-125)。 2·5 μg、5 μg 和 10 μg 组的年轻人分别有 128 (95–173) 和 129 (99–169) 例,相应的数字分别为 99 (70–139)、99 (69– 144) 和 120 (84-172) 在老年人中;在年轻人的 2 期试验中,5 μg 第 0 天和 14 天组的 GMT 为 20 (14–27),第 0 天和第 21 天 5 μg 组中的 GMT 为 53 (38–75),44 (32–61)在 5 μg 第 0 天和第 28 天组中,在 10 μg 第 0 天组中为 7 (6-9) 个。整个疗程后第28天至第90天,中和抗体滴度的GMT下降35·8%(老年人第0天、第28天和第56天10 μg组)至70·8%(10 μg第0天组)接种疫苗;然而,我们没有观察到在接种全过程疫苗后第 90 天接种 3 剂不同剂量的患者的中和抗体的血清转化率有统计学差异,血清转化率为 79·8%(69·6%-87·8%)。 ) 到 91·7% (83·6%−96·6%) 的年轻人和 78·1% (67·5%−86·4%) 到 82·7% (72·7%−90·2) %) 在老年人中。在四个探索性的 2 剂或 1 剂组中,5 μg 第 0 天和 21/28 组的血清转化率为 71·1%(60·1%-80·5%),高于 50·0%( 38·9%−61·1%) 在 5 μg 第 0 天和第 14 天组中和 14·3% (7·6%−23·6%) 在 10 μg 第 0 天组中(补充附录,表 5)。对于特定的 IgG 结合抗体水平,发现了类似的模式。
在全程接种90天后,在年轻人中,2·5 μg, 5 μg, 和 10 μg组中和抗体GMT分别为87 (95% CI, 61–125). 128 (95–173), 129 (99–169)。在老年人中,2·5 μg, 5 μg, 和 10 μg组中和抗体GMT分别为99 (70–139), 99 (69–144), and 120 (84–172)。同样还发现两针间隔时间越长,第二针接种完毕产生的抗体水平更高,在5 μg时,相隔14,21和28天的两针接种完毕,中和抗体GMT分别为20,53,44。
在完全接种28天后至3个月(90天)时,中和抗体滴度明显下降35.8-70.8%;在老年人中,接种5 μg时,从第2针对接种完毕后14天中和抗体浓度达到71,但是在第90天时为54.
Geometric mean titre (95% confidence interval) of antibodies in different time points in the phase 1 trial among participants aged 60 years or older
|
Days 0, 28, and 56 |
||||
|
2·5 μg (n = 24) |
5 μg (n = 24)* |
10 μg (n = 24)† |
Placebo (n = 24) |
|
|
Neutralizing antibodies to live SARS-CoV-2 |
||||
|
Before first dose |
5 (5-5) |
5 (5-5) |
5 (5-5) |
5 (5-5) |
|
4 days after first dose |
5 (5-5) |
5 (5-5) |
5 (5-5) |
5 (5-5) |
|
14 days after first dose |
5 (5-5) |
6 (4-8) |
7 (5-11) |
5 (5-5) |
|
Before second dose |
9 (5-14) |
10 (6-17) |
8 (5-13) |
5 (5-5) |
|
4 days after second dose |
17 (10-32) |
16 (9-28) |
25 (14-45) |
5 (5-5) |
|
14 days after second dose |
86 (46-158) |
71 (36-143) |
102 (68-152) |
5 (5-5) |
|
Before third dose |
90 (48-167) |
54 (29-102) |
89 (61-130) |
5 (5-5) |
|
4 days after third dose |
61 (36-105) |
74 (33-164) |
99 (65-150) |
5 (5-5) |
|
28 days after third dose |
177 (104-302) |
172 (91-328) |
187 (119-295) |
5 (5-5) |
|
90 days after third dose |
110 (62-195) |
106 (50-224) |
118 (68-202) |
5 (5-5) |
|
Specific antibody responses to SARS-CoV-2 |
||||
|
Before first dose |
10 (10-10) |
10 (10-10) |
10 (10-10) |
10 (10-10) |
|
4 days after first dose |
10 (10-10) |
10 (10-10) |
10 (10-10) |
10 (10-10) |
|
14 days after first dose |
15 (12-20) |
13 (11-16) |
16 (12-20) |
10 (10-10) |
|
Before second dose |
15 (12-20) |
19 (16-23) |
17 (13-22) |
10 (10-10) |
|
4 days after second dose |
19 (15-26) |
21 (17-25) |
21 (16-28) |
10 (10-10) |
|
14 days after second dose |
92 (56-153) |
99 (62-159) |
122 (84-177) |
10 (10-10) |
|
Before third dose |
110 (65-184) |
88 (53-144) |
138 (103-183) |
10 (10-10) |
|
4 days after third dose |
120 (74-195) |
91 (59-140) |
126 (98-161) |
10 (10-10) |
|
28 days after third dose |
170 (131-219) |
234 (157-348) |
259 (206-326) |
10 (10-10) |
|
90 days after third dose |
131 (93-184) |
199 (134-296) |
198 (150-261) |
10 (10-10) |
不过,在接种第3剂疫苗时,会诱导强烈的免疫反应,抗体滴度从第3剂起始, 2·5 μg、5 μg 和 10 μg 剂量在老年人中分别为90,54,89,但是第3剂接种后28天分别为177,172,187,不过遗憾的是再过90天,中和抗体滴度下降为110,106,118,同样再次明显下降。不过仍然比第2针结束后90天的浓度要高不少。
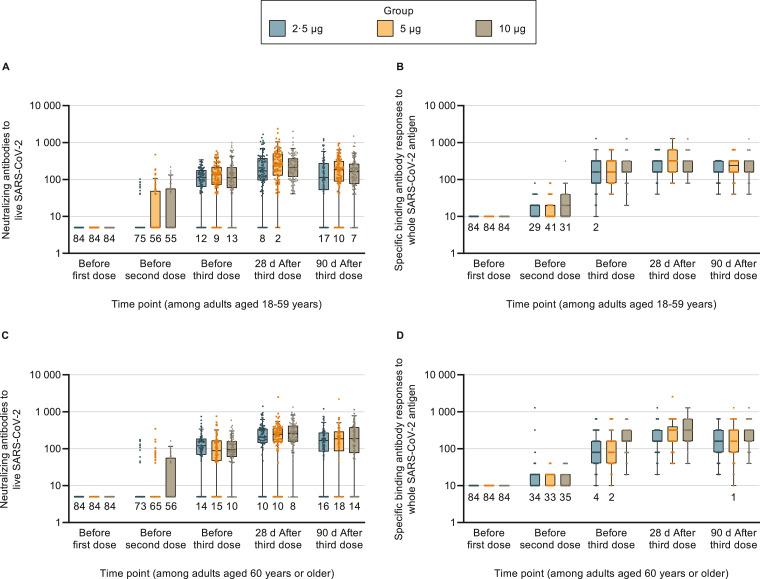
受试者接受第3针时的中和抗体水平
总之,1/2 期试验的初步结果表明,针对 SARS-CoV-2 的灭活疫苗对成年人(包括 60 岁或以上的老年人)是安全且具有免疫原性的。 结果还表明,鉴于与单次高剂量(第 0 天 10 µg)相比具有更好的免疫原性特征,在第 0 天和第 21/28 天的 5 µg 两剂给药方案可以进一步测试其功效在第 3 期试验中的效果。 两剂给药方案,给药间隔较短(第 0 天和第 14 天为 5 µg)。 如预期的那样,第三次加强剂量可能会产生更高的抗体滴度,但这可能会减少可以接种疫苗的人数并导致疫苗供应不足。
梅斯医学小编认为,最近有研究表明,中和抗体滴度直接与疫苗防护相关。从这样的数据来看,第3针似乎难以避免。而且第2针与第3针间隔多少,仍然需要进一步研究。本研究间隔90天,而目前从国内实际情况,即使接种第3针,可能会间隔6个月,甚至以上。第一批接种新冠疫苗的人是在去年底和今年初,至今已过去半年多了。间隔半年,相信中和抗体滴度会更大幅度下降,这就能解释为什么南京疫情快速传播的原因了。此时,如果接种第3针,中和抗体水平会上升多高,值得再次研究。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#CIN#
43
#DIC#
49
#体能#
64
#疫苗接种#
35
#clinical#
44
#Medicine#
43
#Med#
27
努力!
63
学习学习
71
学习学习
80