Blood:FLT3抑制剂Gilteritinib vs 挽救化疗对复发/难治性AML患者长期预后的影响
2022-02-27 Nebula MedSci原创
Gilteritinib维持治疗可保持复发性/难治性AML患者获得持久的缓解
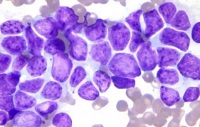
靶向治疗的出现增加了新确诊的复发性或难治性 (R/R) 急性髓系白血病(AML)患者的治疗选择。与单纯化疗相比,抑制FLT3激酶活性的药物 (单用或与化疗联合使用) 明显提高了AML患者的生存率和缓解率。
随机化的3期ADMIRAL试验对比了Gilteritinib和挽救化疗在FLT3突变阳性(+)的复发性或难治性AML患者中的疗效。在该试验中,受试患者被随机(2:1)分至Gilteritinib组(120 mg/天)或挽救化疗组。
ADMIRAL的初步分析显示,Gilteritinib相比挽救化疗可显著延长受试患者的总生存期(9.3个月 vs 5.6个月;死亡风险比[HR] 0.64,p<0.001)。
但是,ADMIRAL试验进行初步分析时的随访时间较短,限制了对长期预后的评估。因此,研究人员对ADMIRAL试验进行了延长随访,本文汇报了自初始分析后又随访了两年的疗效和安全性结果。
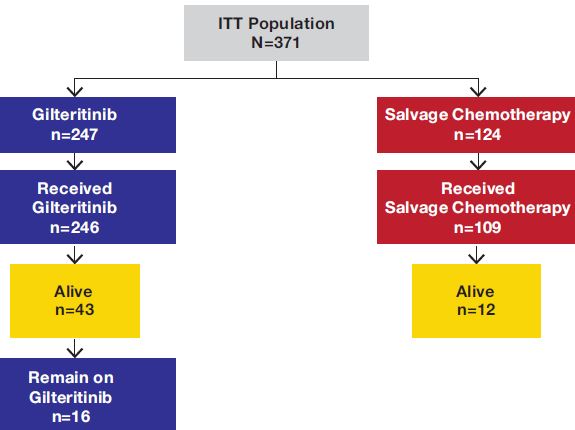
研究流程
截止本次分析时,中位随访了37.1个月,Gilteritinib组和挽救化疗组分别有203例(总人数247位)和97例(总人数124位)死亡;Gilteritinib组有16位患者仍在接受治疗。Gilteritinib组和挽救化疗组的中位总生存期分别是9.3个月和5.6个月(HR 0.665, p=0.0013);两年预计生存率分别是20.6%和14.2%。
两组的总生存率
Gilteritinib组的两年累积复发率分别是75.7%,随访18个月后复发就较少发生。总体上,Gilteritinib组247位患者中有49位、挽救化疗组124位中有14位存活时间达到了两年及以上。Gilteritinib组有26位患者存活两年及以上且无复发;其中18位患者进行了造血干细胞移植(HSCT),16位在HST维持治疗后又开始了Gilteritinib治疗。
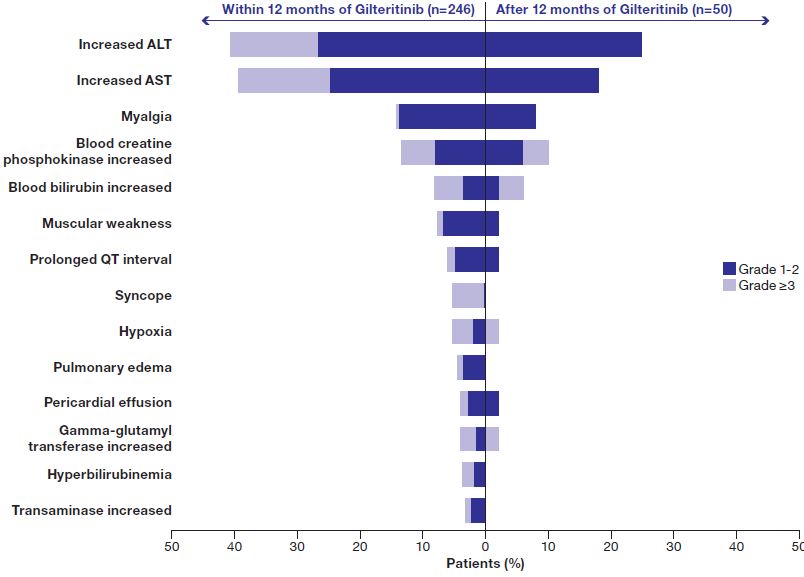
副作用
最常见的副作用是肝酶升高。
总而言之,Gilteritinib维持治疗可保持复发性/难治性AML患者获得持久的缓解,且具有稳定的安全性。该研究结果证实了延长Gilteritinib治疗是安全的,且与S挽救化疗相比具有更好的生存率。
原始出处:
Alexander E. Perl, et al. Follow-up of patients with R/R FLT3-mutation-positive AML treated with gilteritinib in the phase 3 ADMIRAL trial. Blood blood.2021011583. https://doi.org/10.1182/blood.2021011583
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#抑制剂#
31
#长期预后#
40
#Gilteritinib#
28
#难治性#
32
#FLT3#
37
#FLT3抑制剂#
44
AML的**
70