JPD:下丘脑核团的结构连接改变,和冻结步态的息息相关
2022-05-23 Freemann MedSci原创
STN-DBS可以通过调节与前额叶和运动皮层结构相连的特定通路来减轻FOG的严重程度
步态障碍如步态冻结(FOG)是帕金森病(PD)患者的高致残性症状,影响生活质量、发病率和独立性。FOG患者尽管有意行走,但会突然出现无效的步态,通常被认为是 "粘在地上"。

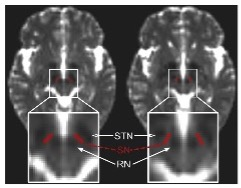
图1: 论文封面图
当FOG发生在OFF状态时,但可以通过多巴胺能药物治疗得到缓解,这被称为 "左旋多巴反应性冻结 "或 "OFF冻结",而 "左旋多巴无反应性冻结 "对多巴胺能药物治疗的变化无动于衷,甚至可以通过药物治疗恶化为 "ON冻结"。
虽然丘脑下核(STN)的深部脑刺激(DBS)是治疗严重PD运动症状的既定方法,但其对步态困难和FOG的影响一直被讨论得很有争议。此外,皮层刺激方案,如重复经颅磁刺激多个目标,已被引入治疗PD的FOG。 不同的潜在解剖学目标的存在表明,更广泛的网络参与了FOG的治疗,这与目前关于其病理的网络模型是一致的。值得注意的是,FOG通常被理解为一种复杂的综合征,超越了纯粹的运动角度。
相反,一系列的成像研究表明,至少在一些患者的认知甚至边缘回路可能在FOG的出现中进一步发挥关键作用。这种多网络的观点与现象学观察相吻合,即FOG的触发因素可以分为运动(如转弯)、认知(如多任务)或边缘触发(如焦虑)。
因此,FOG被认为是由运动、认知或边缘输入到中脑运动区的信号失调导致的,干扰了步态期间的自动运动。这种多网络的观点表明,平均而言,FOG可能通过调节运动、认知和潜在的边缘通路来改善。
藉此,德国科隆大学的Daniel H. Lencha等人,假设STN-DBS通过调节基底神经节内的特定回路来缓解FOG,反映了运动、认知和边缘功能。其次,假设与间脑运动区的结构连接也是这个有益网络的一部分。
他们探究了47名PD和术前FOG的患者。主要使用步态冻结问卷(FOG-Q)来评估冻结的发生率和严重程度。在18名患者的子集中,评估了标准化步行过程中的诱发FOG。通过使用一个公开的基底神经节通路模型,他们确定了与术后FOG变化有关的刺激依赖性连接。使用疾病特异性规范连接组,对先验定义的间脑区域进行了兴趣区域分析。
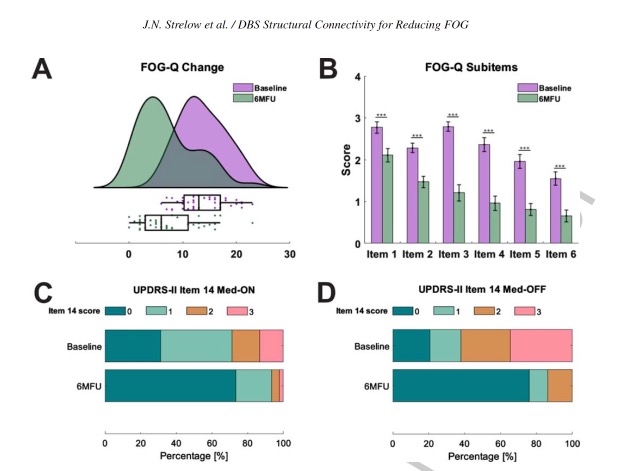
图2:论文结果图
他们发现:术后6个月步态冻结明显改善,标志是冻结发作的频率和持续时间减少。
改善FOG的最佳刺激量在结构上与运动区、前额叶皮层和球状体相连。
这种连通性特征在留置交叉验证中是强有力的。
在皮层下,对穿越小脑幕核和黑质的纤维的刺激与术后改善有关。
该研究的重要意义在于发现了: STN-DBS可以通过调节与前额叶和运动皮层结构相连的特定通路来减轻FOG的严重程度。更加分化的FOG评估可能允许在未来区分特定FOG亚型的通路。
原文出处:
Strelow JN, Baldermann JC, Dembek TA, et al. Structural Connectivity of Subthalamic Nucleus Stimulation for Improving Freezing of Gait. _JPD_. Published online April 11, 2022:1-17. doi:[10.3233/JPD-212997](https://doi.org/10.3233/JPD-212997)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言



















#步态#
38
#冻结步态#
49
#下丘脑#
46
#丘脑#
38
#丘脑#
48