ASCO 2021: 摘要概览与展望 16 |ctDNA在预测结直肠癌复发及全程管理中的潜在作用
2021-05-31 K.K MedSci原创
2021年ASCO上,公布了用ctDNA检测评估结直肠癌患者的复发风险的结果。
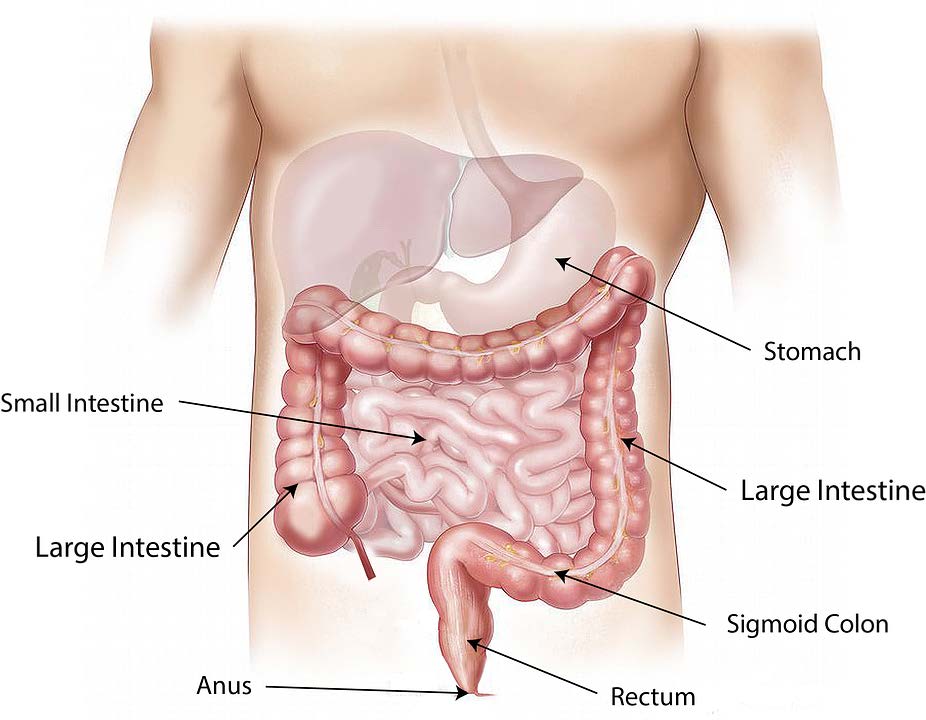
目前大肠癌(CRC)治疗的主要挑战,是能够及时发现患者术后复发,并识别出经手术及辅助治疗(ACT)后,具有高危复发风险的患者。循环肿瘤基因(循环肿瘤DNA),即ctDNA( circulating tumor DNA),是指肿瘤细胞体细胞DNA经脱落或者当细胞凋亡后释放进入循环系统,是一种特征性的肿瘤生物标记。通过ctDNA检测,能够检出血液中的肿瘤踪迹,可用于识别微小残余病变(MRD)和高风险复发性患者。
2021年ASCO上,公布了用ctDNA检测评估结直肠癌患者的复发风险的结果。
这项前瞻性多中心的研究目的是为了确定多次手术后,使用ctDNA检测是否能识别高风险复发性患者、比标准的放射性核素成像更早发现复发病,同时评估辅助治疗。
该队列研究包括了265名临床I-III期结肠直癌患者,也是迄今为止评估ctDNA检测的一项最大队列。这些患者都切除了肿瘤,其中62.6%(166/265)患者接受了辅助治疗(ACT)。
在不同的时间点收集血浆样本(n = 1503),随访时间中位时间为28.4个月。对每个肿瘤和匹配的胚系DNA进行全外显子测序,并鉴定了体细胞单核苷酸变异(SNVs),设计了个性化的多重PCR检测,以追踪每位患者血浆样本中的肿瘤特异性SNVs。
在ACT治疗前,对218名患者进行了术后ctDNA检测,其中9.17%(20/218)被确诊为血液病微小病灶残留(MRD)阳性,75%(15/20)的患者疾病复发,余下25%(5/20)的MRD阳性患者未复发,后接受了ACT治疗。相比之下,只有13.6%(27/198)的MRD阴性病例复发(HR:11:95%CI:5.7-20;p<0.001)。纵向ctDNA阳性指的是治疗后(n = 202)与HR 36(95% CI:16-81;p < 0.001)有关。
对155名术后患者进行了癌胚抗原(CEA)和ctDNA的评估比较,其中发现与CEA相比,ctDNA阳性状态与无复发生存期显著相关。无复发生存期(recurrence-free survival,RFS)的定义是指初次手术至最早出现复发证据的时间。多次ctDNA检测到MRD的中位数为8个月,早于放射性核素成像。
与CEA相比,术后ctDNA阳性状态与RFS明显降低有关。研究还显示,有效治疗可以治愈部分MRD阳性患者。纵向研究显示,ctDNA分析可以预测复发风险,是监测治疗反应更可靠的生物标志物。
总的来说,纵向ctDNA分析的意义:1、能够对CRC患者进行残余病灶检测和复发风险分层;2、潜在地改变 CRC术后管理,使早期复发检测和临床复发的早期发现成为可能;3、评估ACT的有效性,包括指导ACT患者的选择,指导ACT时间的优化成为可能。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#ASC#
43
#ASCO2021#
95
学习了
65
#结直肠#
44
#全程管理#
43
ctdna对复发有指导意义
57
学习了
69