强直性脊柱炎(AS)当中的“炎”,是机体先天免疫系统(抵御疾病和损伤的第一道防线)的一部分,但如果炎症反应持续的时间过长,就会导致一种被称为慢性炎症的疾病(这种情况下,机体会攻击自我,对器官和系统造成破坏),典型的表现是红、肿、热、痛和功能障碍。非甾体抗炎药就是强直性脊柱炎患者常见的“抗炎”用药之一。
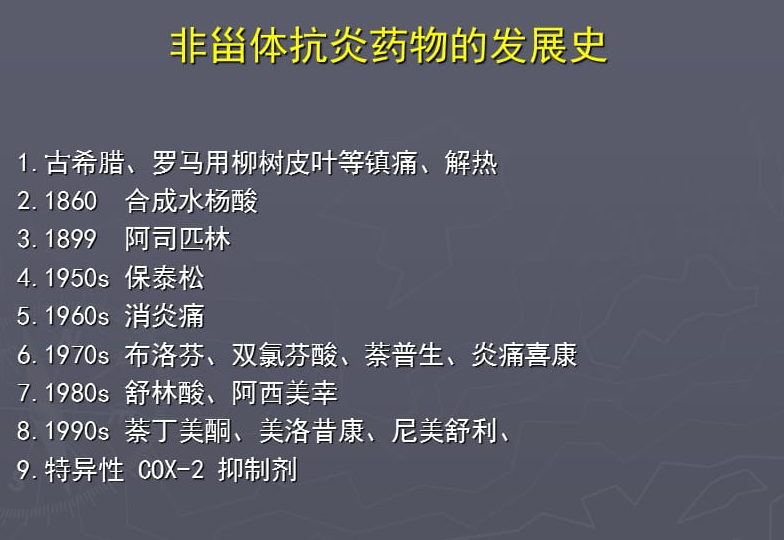
甾体通常是指类固醇类物质(即我们理解的激素),而非甾体类抗炎药(NSAIDs),则是指非激素类的抗炎药物。
临床中经常用到的阿司匹林、吲哚美辛、萘普生、布洛芬、双氯芬酸、洛索洛芬、美洛昔康、塞来昔布、依托考昔、帕瑞昔布都属于非甾体抗炎药。
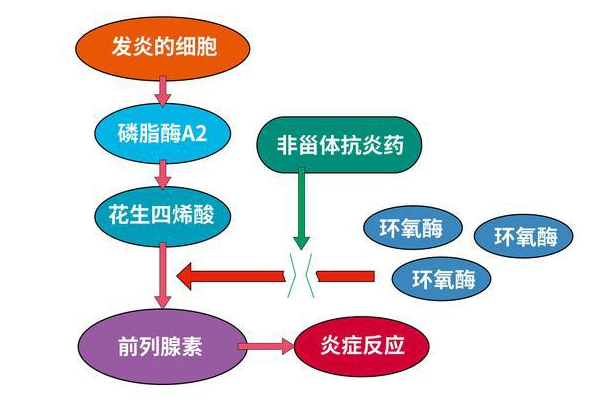
强直性脊柱炎患者常见的炎症介质包括前列腺素、白细胞介素和肿瘤坏死因子等等,这些炎症介质是强直性脊柱炎疼痛的罪魁祸首。通过药物抑制炎症介质时,可以缓解炎症,同时也可以减轻疼痛。非甾体抗炎药(NSAIDs)正是这样一种药物,它作用于环氧化酶,抑制花生四烯酸合成前列腺素,从而抑制炎症,减轻疼痛。
但需要注意的是,强直性脊柱炎还有一个显著的特征——新骨形成。强直患者骶髂关节可以出现骨质破坏和骨性融合,脊柱受累可伴随包括肌腱韧带、椎间盘、终板及骨突结构在内的异位骨化,韧带骨赘从相邻椎骨生长,最终相连形成新生骨桥,形似竹节样改变。这些病理变化进一步影响身体机能,严重降低生活质量,最终导致残疾。因此,抑制新骨形成具有重要意义。
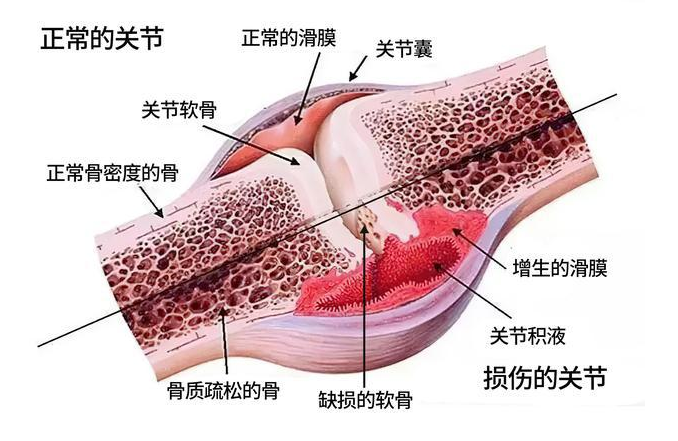
而非甾体抗炎药因对于关节腔深层炎症控制的效果有限,对局部软组织粘连“束手无策”,因此难以阻止骨赘的形成,所以对于中晚期强直患者来说,单一使用非甾体抗炎药就很难控制病情。这和药物本身关系不大,而是局部问题的复杂性,已经超出了药物的作用范畴。
和其他任何药物一样,非甾体抗炎药在发挥治疗效果的同时,长期使用,也会产生一些不良反应。非甾体抗炎药的不良反应主要表现在以下多个方面。
01胃肠道
可出现上腹不适、隐痛、恶心、呕吐、饱胀、嗳气、食欲减退等消化不良症状。长期口服非甾体抗炎药的患者中,10%~25%可能发生消化性溃疡,其中有小于1%的患者出现严重的并发症如出血或穿孔。
02肝脏
在治疗剂量下,10%的患者出现肝脏轻度受损的生化异常,但谷丙转氨酶指标明显升高的发生率低于2%。
03神经系统
可出现头痛、头晕、耳鸣、耳聋、弱视、嗜睡、失眠、感觉异常、麻木等。有些症状不常见,如多动、兴奋、幻觉、震颤等,发生率一般小于5%。
04泌尿系统
可引起蛋白尿、管型尿,尿中可出现红、白细胞等,严重者可引起间质性肾炎。在一项多中心的临床研究中,长期口服非甾体抗炎药的患者肾脏疾病发生的风险率是普通人群的2.1倍。
05血液系统
部分非甾体抗炎药可引起粒细胞减少、再生障碍性贫血、凝血障碍等。
06过敏
特异体质者可出现皮疹、血管神经性水肿、哮喘等过敏反应。
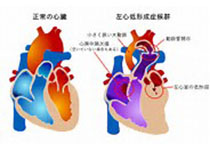
07心血管系统
有研究发现,非甾体抗炎药能明显干扰血压,使平均动脉压上升。另有报道,服用罗非昔布18个月后,患者发生心血管事件(如心脏病发作和中风)的相对危险性增加了。
08妊娠期
非甾体抗炎药被认为是诱发妊娠期急性脂肪肝的潜在因素;孕妇服用阿司匹林可导致产前、产后和分娩时出血;吲哚美辛可能会引起某些胎儿短肢畸形、阴茎发育不全。
① 在临床应用中,应避免联合使用两种及两种以上非甾体抗炎药。
② 存在胃肠道不适或消化性溃疡者,优先选择COX-2抑制剂而非传统非甾体抗炎药,必要时加用胃药。
③ 对于仅有心血管高风险,而无其他风险因素的患者,考虑优先使用萘普生。
④ 在应用非甾体抗炎药治疗的同时,如情况允许注意避免使用利尿剂、ACEI/ARB类降压药等可能同时影响肾脏灌流的药物。
⑤ 非甾体抗炎药具有封顶效应,应避免超剂量用药。过量用药,疗效不增加,但是副作用会显著增加。
⑥ 应在医生指导下,定期进行必要的血液、肾功能监测。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#塞来昔布#
60
#非甾体抗炎药#
63
#抗炎药#
47
#吲哚美辛#
59
学习了。
71
优秀
57