Genome Biol:开发出有望识别致癌病原体的新方法
2019-11-08 佚名 细胞
近日,一项刊登在国际杂志Genome Biology上的研究报告中,来自东英吉利亚大学等机构的科学家们通过研究开发了一种新方法来寻找与癌症相关的细菌和病毒。
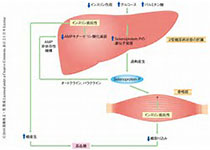
如今研究人员已经发现,某些感染与癌症发生直接相关,比如胃癌和宫颈癌等;这项研究中,研究者通过研究揭示了如何对来自肿瘤的基因组数据进行测序来揭示与其发生相关的细菌和病毒,相关研究结果或能帮助检测致癌微生物,未来有一天或能帮助开发多种癌症疫苗,比如HPV疫苗等。
研究者Dan Brewer博士说道,某些感染与癌症发生存在明显关联,比如,消化道中幽门螺杆菌的存在就会引发胃溃疡,并与胃癌发生直接相关;某些类型的HPV也会引发宫颈癌;随着人类进入到基因组医学时代,如今研究人员对人类组织进行全基因组测序的工作也越来越多,当对肿瘤样本进行全基因组测序时,来自任何病原体的DNA也能够被进行测序,这就有望帮助研究者检测和定量病原体。
因此,研究人员就能利用所收集的数据来识别细菌、病毒和不同类型癌症之间的关联;文章中,研究人员开发了计算机模拟技术,当对真正的癌症测序数据进行分析之前,其能对多种方法就进行验证,并在这些数据中寻找一些有趣的病原体;在模拟实验中,研究人员制造了包含大部分人类基因组序列的“模拟”基因组,同时还在其中加入了少量的病原体序列,而这正是研究人员希望在癌症序列中所观察到的。
当研究者在每一个模拟的基因组中发现病原体并对其进行定量分析后,他们就能够检测每一种方法是否可行;研究者除了发现与癌症发生相关的病原体外,他们还能够发现更多病原体,目前研究人员才刚刚开始研究确定这些病原体在癌症发生过程中所扮演的关键角色。最后研究者Brewer表示,如今人们所注射的HPV疫苗能够有效预防大约70%的宫颈癌病例,我们希望后期能够通过更为深入的研究识别出与其它癌症发生相关的细菌和病毒,从而开发出有效预防癌症发生的新型疫苗。
原始出处:
Abraham Gihawi, Ghanasyam Rallapalli, Rachel Hurst, et al. SEPATH: benchmarking the search for pathogens in human tissue whole genome sequence data leads to template pipelines, Genome Biology (2019). DOI:10.1186/s13059-019-1819-8
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Bio#
30
#Biol#
36
#新方法#
34
#致癌#
27
#病原体#
34