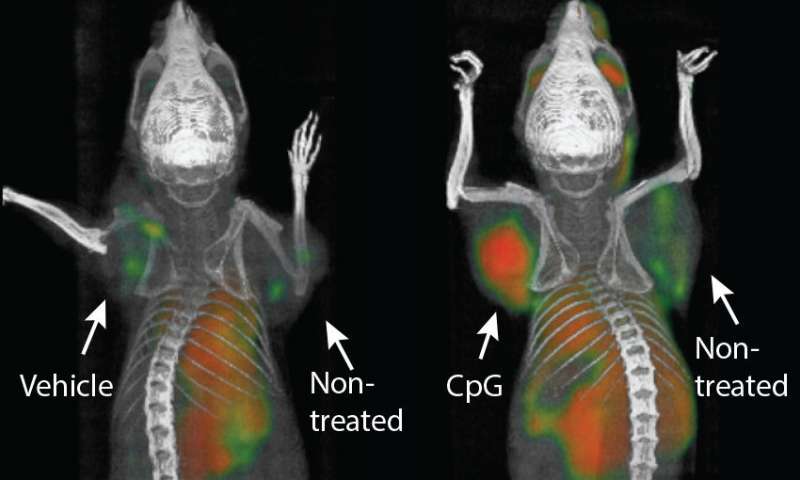
Cell Stem Cell:这是真正的防癌疫苗!科学家用诱导性多能干细胞研发新型疫苗,能“团灭”轮番入侵的癌细胞
2018-02-28 应雨妍 奇点网
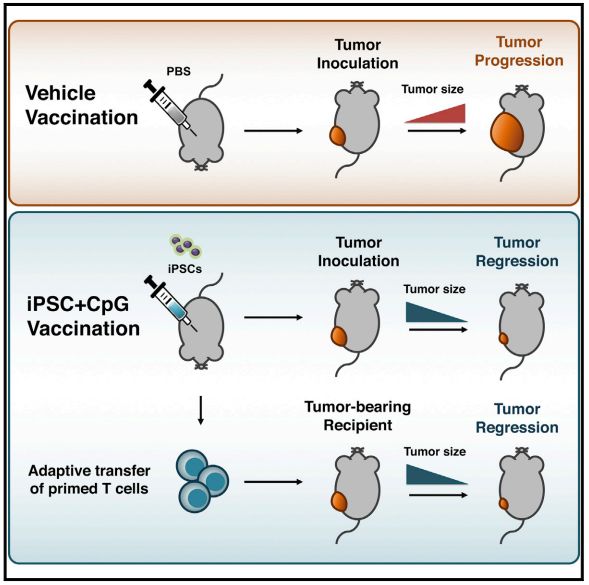
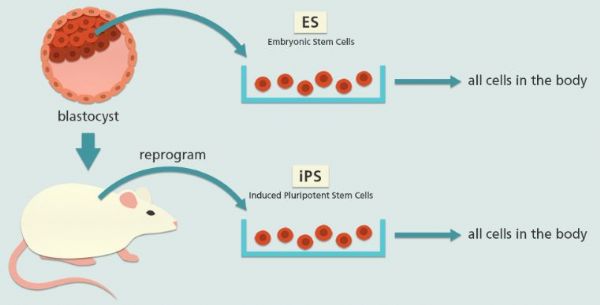
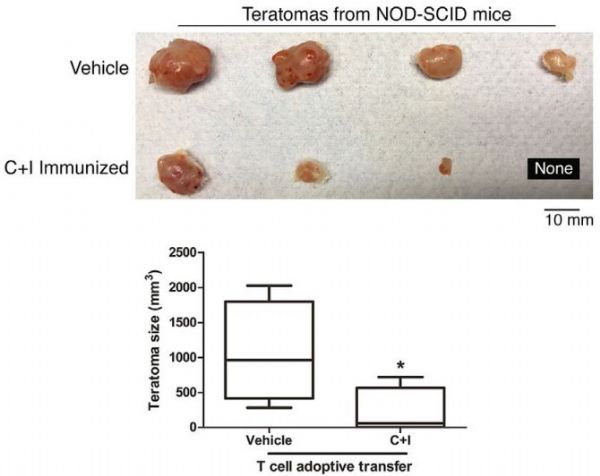
“癌症疫苗”,一直是领域内许多研究人员的梦想。我们现在所见的癌症疫苗一般都是“治疗性疫苗”,通过增强免疫系统攻击肿瘤的能力,减小、甚至消灭肿瘤。然而这和我们认知中的疫苗不太一样,从小到大,我们接种的都是预防性疫苗,将疾病扼杀在摇篮中的那种,那癌症能不能也这样呢?

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#stem cell#
47
#Cell#
33
#CEL#
42
#诱导性#
39
学习了谢谢分享!!
80
#癌细胞#
28
#研发#
31
#STEM#
0
#防癌#
35
学习了
73