【一般资料】
患儿,男,3岁,92cm,13kg,
【现病史】
因“先天性心脏病,法洛四联症,体肺分流术后,声门下狭窄”拟行声门下狭窄松解术。患儿出生后40d,因咳嗽就诊,心脏彩超示“先天性心脏病,法洛四联症”,肺动脉及左心室发育差,于我院行体肺分流术。术后1年肺动脉及左室发育尚好,欲行法洛四联症根治术。术中喉镜示声门下环形狭窄,气管插管困难,取消手术。
【体格检查】
患儿本次于2015年入院后,监测吸纯氧条件下SpO285%~90%,步行50m出现气喘,口唇发绀。
【辅助检查】
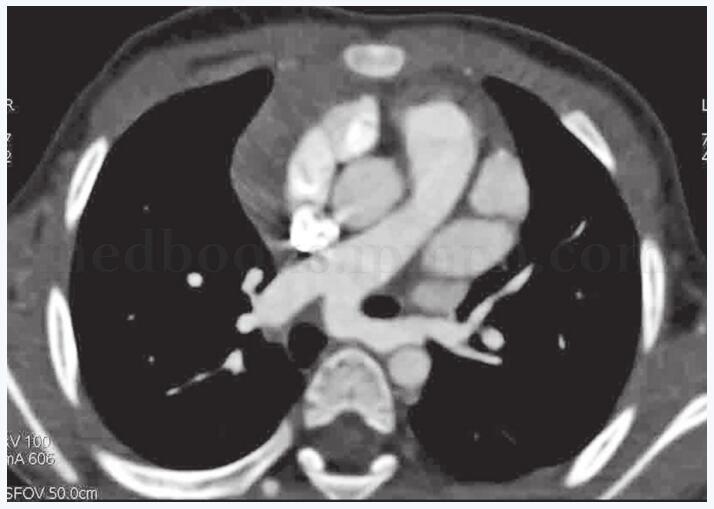
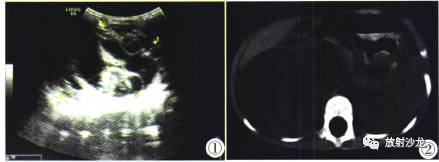
CT增强扫描示:右室横截面积3.1~4.8cm2,右室壁增厚,左室体积与右室相当;室间隔缺损直径约0.7cm,肺动脉发自右心室,右室流出道狭窄,最窄处直径约0.5cm,肺动脉瓣环狭窄,瓣叶增厚;主动脉骑跨,骑跨率为50%,升主动脉右侧可见管状连接于右肺动脉。颈椎CT示:主气管局部环形狭窄,狭窄长度约2.2mm,最窄处直径4.6mm。其他辅助检查未见异常。
【治疗】
术前全院会诊拟定气管插管全麻,备用方案为“保留自主呼吸下静脉麻醉并保证气道通畅高氧大流量给氧”,拟行声门下狭窄松解术。患儿入室前肌注40mg氯胺酮,监测ECG、NIBP、SpO2,行桡动脉穿刺监测ART,开放静脉通路,吸氧去氮3min,麻醉诱导静注咪达唑仑1mg、舒芬太尼5μg、地塞米松5mg、东莨菪碱0.15mg、琥珀胆碱70mg,1%丁卡因充分舌根声门表麻,后试插ID4管两次失败,吸氧,改插ID3.5管失败。诱导开始10min后自主呼吸逐渐恢复,为防止气道水肿加重狭窄程度,放弃插管,改为保留自主呼吸条件下静脉浅麻醉并保证气道通畅、高氧大流量给氧,术者在支撑喉镜下行手术。方法:将ID3.5气管导管直接退回至口腔,维持纯氧浓度,氧流量8L/min。术中保证血氧维持于75%~85%,间断面罩辅助通气。手术时间35min,NIBP80~120/45~80mmHg,HR75~115次/分,SpO275%~93%。术中血气回报间断给予碳酸氢钠50ml纠酸及对症处理,为防止插管创伤及术后气管水肿,给予甲基强的松龙40mg。术毕总计液体转化糖电解质入量120ml,为防止术后气管再度狭窄,插管ID5管顺利通过,深度17cm越过声门下最细处4.6mm的膜性狭窄,术毕血气pH7.198,PCO254.3mmHg,PO275mmHg,HCO-323.2mmol/L转ICU继续观察。术后随访,患儿入ICU清醒后拔管,无明显不适,等待法洛四联症根治术。
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#气道管理#
48
#法洛四联症#
35
#全麻#
32
非常好的文章.学习了
53