Endocrinology:生长激素会促进衰老,破坏脂肪中的生长激素受体,可延长寿命
2022-10-27 王聪 “生物世界”公众号
大量证据表明,在哺乳动物中,生长激素作用的减少与衰老减缓相关(包括衰老相关关键通路的信号减少、寿命增加、年龄相关疾病减少等等)。
生长激素的最重要作用是调节生长,然而,它的存在既有好处也有坏处。生长激素存在于人体的许多组织中,在包括衰老在内的许多生物功能中发挥着重要作用。
大量证据表明,在哺乳动物中,生长激素作用的减少与衰老减缓相关(包括衰老相关关键通路的信号减少、寿命增加、年龄相关疾病减少等等)。
1997年,俄亥俄大学的 John Kopchick 实验室创造了一种生长激素受体基因被完全和特异性敲除的小鼠,最终,这只小鼠成为世界上最长寿的实验室小鼠(正常小鼠寿命不超过3年),活了5年差1周时间。
由于这只小鼠全身组织和细胞中都缺少生长激素受体,因此无法受到生长激素作用,显得又瘦小又虚胖。如果选择性地只破坏脂肪细胞中的生长激素受体,而不影响其他组织,是否可以既延长寿命,又不产生其他有害影响呢?
近日,俄亥俄大学的的 John Kopchick 等人在 Endocrinology 期刊发表了题为:Disruption of Growth Hormone Receptor in Adipocytes Improves Insulin Sensitivity and Lifespan in Mice 的研究论文。
这项研究显示,只特异性敲除脂肪组织中的生长激素受体基因,可以改善小鼠健康、延长其寿命。

这项研究是建立在 John Kopchick 实验室之前构建的小鼠模型的基础上,他的实验室之前构建了生长激素受体基因敲除小鼠(GHRKO),这些小鼠体内没有生长激素作用,胰岛素敏感性增强、寿命更长,并且能够预防多种与年龄相关的疾病。1997年至今的25年时间里,这些小鼠一直被用于研究健康衰老。
在这项最新研究中,研究团队构建了只特异性敲除脂肪组织中的生长激素受体基因的小鼠(AdGHRKO),然后让这些小鼠正常生活,并分析脂肪组织中生长激素受体基因敲除是否影响了它们的新陈代谢和寿命。
结果显示,脂肪组织中生长激素受体基因敲除可以改善老龄雄性小鼠的胰岛素敏感性,并延长其寿命。这些小鼠的脂肪量增加,胰岛素、C肽、脂联素、抵抗素的循环水平降低,老年小鼠的肌肉力量有所增强,虚弱程度评分也有所改善。
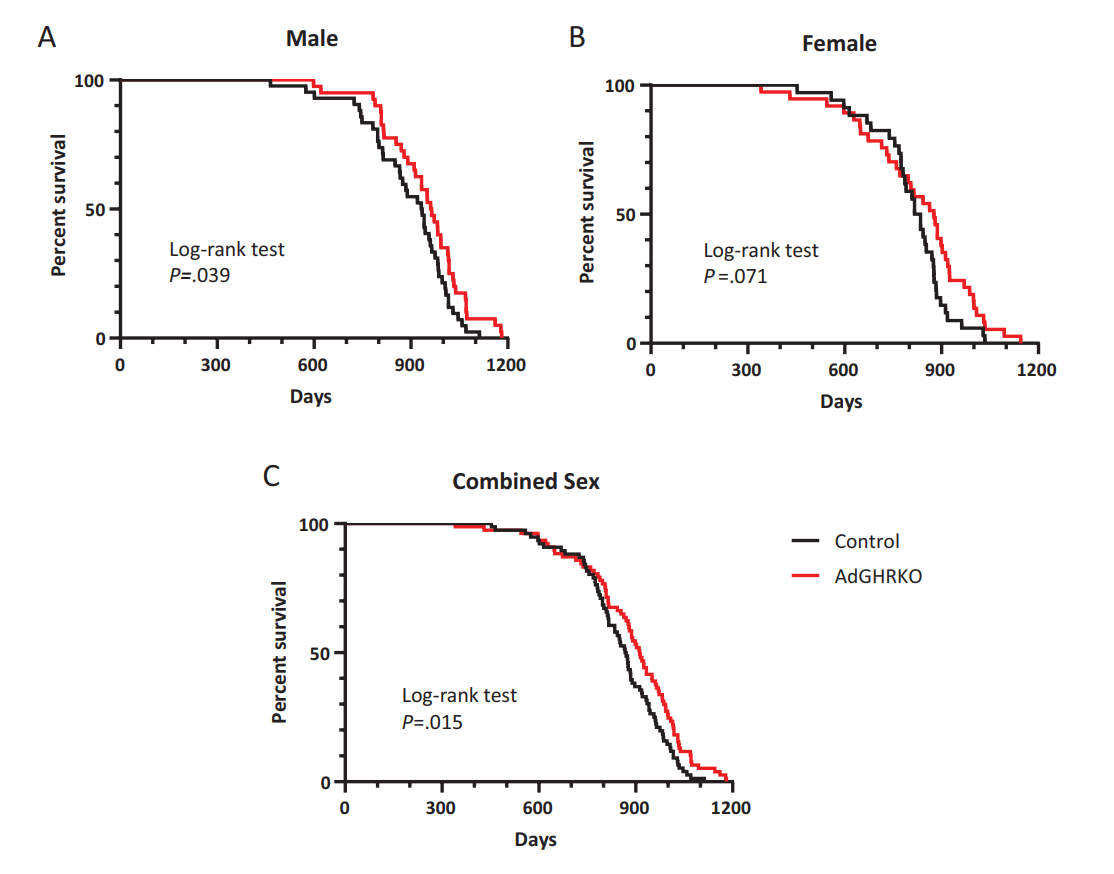
研究团队比较了生长激素受体基因敲除小鼠、脂肪组织生长激素受体基因敲除小鼠和肌肉组织生长激素受体基因敲除小鼠的平均寿命数据。结果表明,生长激素受体基因敲除雄性小鼠的寿命延长,23%得益于脂肪中的生长激素受体基因敲除,19%得益于肌肉中的生长激素受体基因敲除。而雌性从中获益较少,这两个数据分别是19%和0%。也就是说,脂肪组织中敲除生长激素受体基因有助于延长雄性和雌性寿命,但肌肉组织中敲除生长激素受体只能延长雄性寿命。
这些研究结果表明,去除生长激素的作用,即使是在单个组织(脂肪组织)中,也足以产生可观察到的健康效益,促进长期健康,减少虚弱,增加寿命。这项研究也告诉我们,生长激素对健康的一些不利影响发生在脂肪组织中,生长激素并不是一种抗衰老药物,它反而会加速衰老。
John Kopchick 表示,这项新研究扩展了对生长激素的认知,以及它如何影响不同的组织并产生不同的结果。在这项研究中,虽然小鼠的脂肪增加了,但它们的新陈代谢很健康,相比对照组小鼠寿命更长,这也提示了我们,并不是所有的脂肪都是坏脂肪。
原始出处:
Edward O List, et al. Disruption of Growth Hormone Receptor in Adipocytes Improves Insulin Sensitivity and Lifespan in Mice. Endocrinology, Volume 163, Issue 10, October 2022, bqac129.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












学习了
47
转发学习
49
感谢分享
37
学习受益
50
签到学习
50