Stroke:强化降血压,是否减缓小血管病进展?
2021-08-18 Freeman MedSci原创
在严重的脑小血管疾病中,强化降压与弥散张量成像或磁共振成像中白质损伤的进展无关
脑小血管疾病(SVD)占缺血性中风的20%,是血管性认知障碍的最常见原因。高血压是SVD的一个主要危险因素,降低血压(BP)与减少SVD的风险有关。然而,对于有症状的SVD患者,应该降低多低的血压还不确定。
一方面,最近的试验报告称,强化降压,将收缩压定在120至125毫米汞柱,与中风患者一级预防中心血管事件的减少和二级预防中卒中风险的降低有关。然而,有人认为,过度降压可能对SVD有害。
在SVD中会出现脑血流减少和脑自动调节功能受损。在自动调节功能受损的情况下,过度降压可能进一步减少脑血流,加速白质损伤和认知功能的恶化。
大脑自动调节功能在严重的SVD患者中尤其受损,他们有融合的白质增生(WMHs)和多发性腔隙性梗塞,因此这类患者被认为特别容易受到过度降压的影响。SPS3试验发现强化降压在认知能力下降率方面没有差异,但许多患者有轻度SVD。
评估SVD干预措施的临床试验设计一直是个挑战。监测认知变化的神经心理学测试对临床试验中经常使用的2至3年的时间段的变化不敏感,只有在更长时间的随访中才能发现变化。磁共振成像(MRI)可作为有用的替代标记(surrogate marker)。
SPRINT-MRI研究报告称,强化降压与减少WMH病变的发展有关,但这是在没有症状的SVD的高血压患者中。弥散张量成像(DTI)对白质结构的变化更敏感,在SVD中与认知的相关性比WMH体积更好。使用DTI,在SVD中不仅可以检测到WMH内的白质异常,还可以检测到T2-MRI上正常出现的白质,DTI异常可以预测长期的痴呆风险。然而,没有多中心的随机临床试验将DTI作为替代标记物。
藉此,剑桥大学的Hugh S. Markus等人,通过PRESERVE试验探究了强化降压是否与DTI评估的白质损伤增加有关。

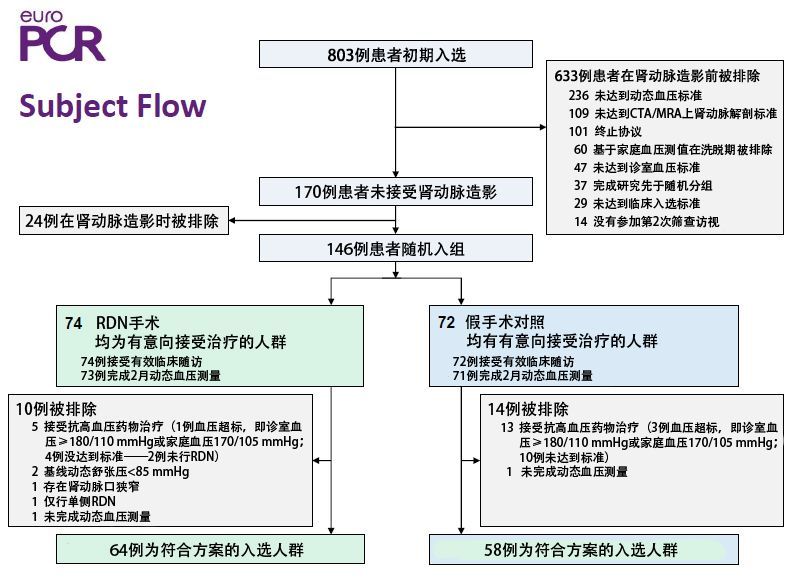
PRESERVE是个随机、平行、多中心对照、盲法结果的临床试验。共招募了111名磁共振成像证实有症状的腔隙性脑梗塞和融合性白质增生的参与者,并随机分配到标准(收缩压=130-140毫米汞柱)(N=56)或强化(收缩压<125毫米汞柱)(N=55)血压目标。
主要结果是基线和24个月之间扩散张量成像白质平均扩散率峰值高度( mean diffusivity peak height,MDPH)的变化。次要结果是其他磁共振成像标志物和认知能力。
纳入的患者平均年龄为68岁,60%为男性。标准组/强化组的平均(SD)血压分别降低了-15.3(15.4)和-23.1(22.04)mmHg(P<0.001)。
MDPH,在两组之间没有差异:标准组,调整后的平均值(SE)=12.5×10-3(0.2×10-3);强化组,12.5×10-3(0.2×10-3),P=0.92。
在24个月的随访中,整个人群的白质微结构明显恶化,但认知能力没有明显下降。
这个研究的重要意义在于发现了:在严重的脑小血管疾病中,强化降压与弥散张量成像或磁共振成像中白质损伤的进展无关。在一项为期2年的多中心研究中,多模态DTI成像对检测变化比认知测试更敏感。
原文出处:
Markus HS, Egle M, Croall ID, et al. PRESERVE: Randomized Trial of Intensive Versus Standard Blood Pressure Control in Small Vessel Disease. Stroke. 2021;52(8):2484-2493. doi:10.1161/STROKEAHA.120.032054
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















怎么能获得原文
42
#小血管病#
42
#血管病#
30
#强化降血压#
30
nice
67