JCO:高复发/死亡风险的前列腺癌患者根治性切除术后或可采用辅助放疗巩固
2021-06-07 Nebula MedSci原创
pN1期或pGleason评分8-10分和pT3/4期的前列腺癌患者,或可考虑采用辅助放射治疗,有望显著降低其全因死亡风险
在随机对照试验中,与根治性前列腺切除术 (RP) 后的早期挽救性放疗 (sRT) 相比,辅助放射治疗未显示出可降低无进展生存期的潜力。但是,鉴于这些试验可能错过了对根治性前列腺切除术时病理学不良的男性的最佳治疗,这些男性可能不具有充分的代表性或不可忽视的时间偏差。
在该研究中,Derya等人调查了这种可能性。招募了具有不良病理特征的前列腺癌患者(盆腔淋巴结转移阳性[pN1]、pGleason评分8-10分或癌灶侵犯到前列腺之外),评估了辅助治疗对比早期挽救性放疗对全因死亡(ACM)风险的影响。在估计辅助治疗与早期挽救性放疗对全因死亡风险的因果影响时,研究人员使用了治疗倾向评分来最小化潜在的治疗选择偏差,同时采用敏感性分析评估不良病理学的不同定义对全因死亡风险的影响,并根据手术时的年龄、前列腺癌预后因素、部位和术后雄激素剥夺治疗的时间依赖性应用进行校正。
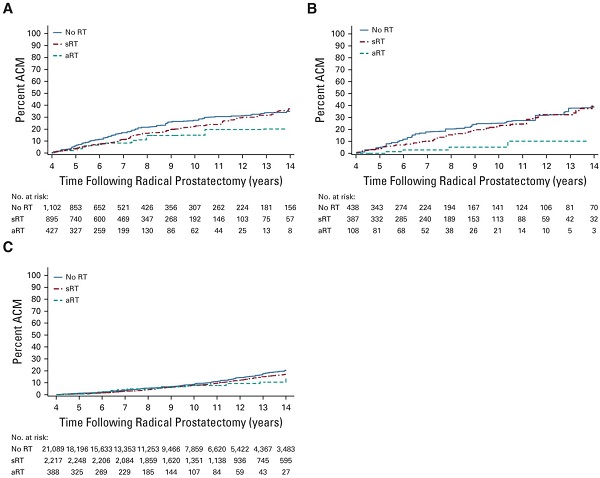
校正的全因死亡风险评估:A)2424位包含pN1期的病理学不良的患者;B)933位不包含pN1期的病理学不良的患者;C)23694位有病理学不良的患者
中位随访8.16年(四分位范围 6.0-12.1年)后,本研究队列共纳入了25118位患者,共有2104位(8.06%)患者死亡,其中539位(25.62%)死于前列腺癌。排除了前列腺特异性抗原持续阳性的患者后,与早期挽救性放疗相比,辅助治疗与根治性前列腺癌切除术时病理性不良的患者显著更低的全因死亡风险相关(0.66[95%CI 0.44-0.99];P=0.04),排除pN1期患者后,该相关性更明显(0.33[0.13-0.85];P=0.02)。
综上,pN1期或pGleason评分8-10分和pT3/4期的前列腺癌患者,或可考虑采用辅助放射治疗,有望显著降低其全因死亡风险。
原始出处:
Derya Tilki, et al. Adjuvant Versus Early Salvage Radiation Therapy for Men at High Risk for Recurrence Following Radical Prostatectomy for Prostate Cancer and the Risk of Death. Journal of Clinical Oncology. June 04, 2021. https://ascopubs.org/doi/full/10.1200/JCO.20.03714
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#切除术#
46
#JCO#
36
ARTvs eSRT
84
#死亡风险#
55
#根治性切除术#
45
#辅助放疗#
73
#根治#
39
#积分#不错
151
前列腺癌相关研究,学习了,谢谢梅斯
61
很好 不错。。。。
63