靶向VEGF / DLL4的双特异性抗体TR009 / ABL001治疗消化道肿瘤,临床前结果喜人
2021-01-07 Allan MedSci原创
TR009表现出比仅针对VEGF或DLL4的单克隆抗体更有效的体外和体内生物学活性。
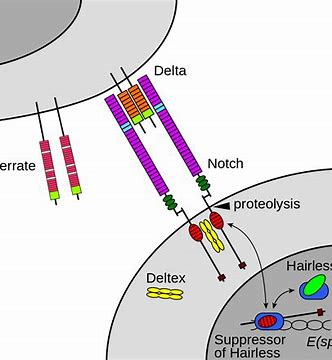
抗新生血管治疗是实体肿瘤治疗中的有效策略,近年来抗VEGF治疗出现了耐药现象。Notch信号转导是一种细胞间信号通路,在肿瘤新生血管生成中起重要作用。在Notch通路中,Delta样配体4(DLL4)在影响肿瘤新生血管生成方面起着重要的作用,它能抑制新生血管分支形成,促进新生血管的成熟。
生物制药公司TRIGR Therapeutics今天宣布,已在《International Journal of Molecular Sciences》上发表了TR009的临床前结果,TR009是该公司针对VEGF / DLL4开发的抑制肿瘤新生血管的双特异性抗体。
结果显示,TR009表现出比仅针对VEGF或DLL4的单克隆抗体更有效的体外和体内生物学活性。此外,TR009与紫杉醇和伊立替康的组合在人胃癌和结肠癌异种移植模型中能够协同抑制肿瘤进展。肿瘤血管的免疫组织化学分析显示,经TR009处理后,肿瘤内皮细胞中VEGFR-2和DLL4(TR009的双重靶标)的表达水平显著降低。与先前的研究一致,数据强烈支持VEGF / VEGFR信号传导与肿瘤脉管系统中的DLL4 / Notch信号通路的相互作用。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#特异性#
40
双特异性抗体是热点,但是也不一定都有效!
73
#VEGF#
42
#消化道#
43
#特异性抗体#
44
#消化道肿瘤#学习了
139
好文章
94