CSH重磅发布:伊布替尼一线治疗CLL研究RESONATE-2发布55个月随访结果
2018-10-29 佚名 肿瘤资讯
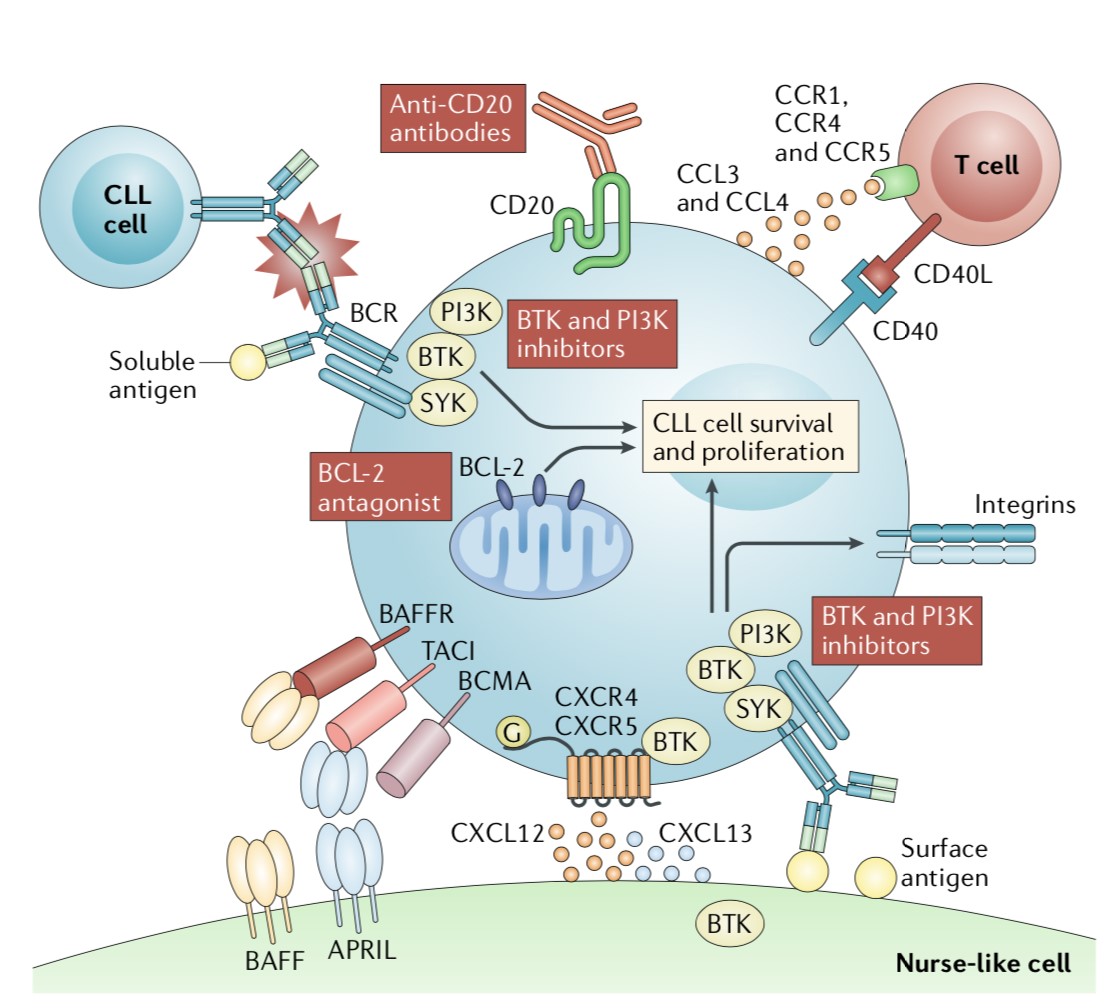
RESONATE-2是当前唯一一项具有长期随访数据的全球、多中心、大规模、III期BTK抑制剂治疗CLL/SLL的随机对照研究,旨在探讨伊布替尼一线治疗CLL/SLL的疗效与安全性。该研究的随访结果持续在ASH、EHA等重要学术会上公布,备受临床专家关注。2018年10月25-28日,中华医学会第15次全国血液学学术会议期间,美国MD Anderson的Jan A. Burger教授公布了RESO
Jan A. Burger终身教授,德克萨斯大学MD安德森癌症中心癌症医学系白血病科终身教授,德国弗莱堡Albert-Ludwigs大学医学院内科学教授,德克萨斯大学休斯顿健康科学中心生物医学研究生院教授,机构研究资助计划下基础研究项目研究部分的审查委员会,UT生物医学研究所实验疗法研究生项目,成员
多学科研究咨询委员会(MRAC),审稿人和成员,伊布替尼作为首创的BTK抑制剂,是当前淋巴瘤治疗最为重要的靶向药物之一,问世以来备受全球临床医生的关注。 伊布替尼自去年11月进入中国市场以来,为中国慢性淋巴细胞性白血病/小淋巴细胞性淋巴瘤(CLL/SLL)的治疗翻开了新的篇章。
今年10月10日,中国国家医疗保障局公布的名单中,将伊布替尼纳入医保报销目录,极大地降低了患者的药物花费。同时,也使得各地的血液淋巴瘤医生对伊布替尼的相关疗效与安全性等信息更为关注。
伊布替尼当前国内获批适应证及医保报销适应证包括:1.既往接受过一种治疗的套细胞淋巴瘤(MCL)患者的治疗;2.慢性淋巴细胞白血病/小淋巴细胞淋巴瘤(CLL/SLL)患者的治疗。
本次中华医学会全国血液学学术会议期间,来自MD Anderson的Jan A. Burger教授通过一项壁报公布了伊布替尼一线治疗CLL/SLL的RESONATE-2研究长达55个月(中位随访4年)的随访结果并受邀在大会期间为中国血液领域医生解读该研究的相关情况。
研究目的
RESONATE-2是一项III期临床研究,旨在比较伊布替尼与苯丁酸氮芥(chlorambuci)一线治疗CLL/SLL患者的有效性及安全性。经独立审查委员会评估的初步结果表明,中位随访18.4个月时,伊布替尼将疾病进展(PD)或死亡风险降低了84%(P <0.001)(Burger,NEJM 2015)。
研究方法
按照1:1,研究人员将269例先前未接受治疗的CLL/SLL患者(年龄65岁以上)随机给予每天1次420mg的伊布替尼或最多12周期的苯丁酸氮芥治疗。主要终点是IRC评估的无进展生存(PFS)。次要终点包括总体反应率(ORR)、血液学改善率和安全性。长期安全数据集中于伊布替尼治疗组。患者报告的结果包括FACIT-疲劳。苯丁酸氮芥组达到PD的患者可切换至伊布替尼治疗。研究人员评估长期疗效。
研究结果
患者基线特征均衡,大多数患者年龄超过70岁(中位年龄73岁),35%的患者存在肿块,39%的患者存在贫血,65%的患者B2M大于3.5mg/L。在纳入的269例患者中,22%的患者存在del(11q),58%的患者IGHV未突变,53%的患者存在高危特征[包括del(17p),TP53突变,del(11q)和IGHV未突变]。
长达55个月的随访(中位随访4年)显示,在伴del(11q)和不伴有del(11q)的患者中,伊布替尼较苯丁酸氮芥分别降低了97%和81%的疾病进展率或死亡率;在IGHV突变和IGHV未突变的患者中,这一概率分别84%和91%。PFS显着延长,甚至在高危特征患者中如del(11q)和IGHV未突变患者中也存在这一优势。伊布替尼组与苯丁酸氮芥组中位随访48个月时的总生存率分别为86%和76%;CR/CRi率从初步分析时的11%升高至27%。伊布替尼组的ORR高达92%。
在血液学改善方面,相比苯丁酸氮芥组,伊布替尼组的患者在治疗期间获得持续的血液学改善,包括贫血和血小板减少,并且随着时间推移持续获益。在CLL治疗相关的症状方面,伊布替尼组的患者症状改善更明显,这些症状包括体重下降、疲劳、乏力、盗汗、腹痛等。在患者报告结果方面,伊布替尼组患者FACIT-F2和EQ-5D-5L3评估结果得以改善。
在安全性方面,苯丁酸氮芥组中有55%的患者在PD后切换至伊布替尼治疗。伊布替尼组中10%的患者发生了主要的血液学不良事件:第1年5例(1例2级,3例3级,1例4级);第1-2年5例(5例3级);第2-3年1例3级;第3-4年3例2级;无严重不良事件发生。
伊布替尼组中,13%和24%的患者发生了心房颤动和高血压,大多数轻微,无严重的不良反应发生,并且随着治疗时间的推移,其发生率逐渐下降。另外,伊布替尼停药或减低剂量的情况也随时间逐渐减少。整体上,11例患者接受了后续治疗,治疗方案包括氟达拉滨+环磷酰胺+利妥昔单抗(FCR)、苯达莫司汀+利妥昔单抗(BR)、苯达莫司汀、放射治疗等,6例患者在后续治疗中获得PR。
研究结论
经过4年的随访,伊布替尼单药治疗显示出持久的疗效,与苯丁酸氮芥相比,总体的疾病进展或死亡风险降低了86%。并且,伊布替尼显着改善了具有高危预后因素(del11q或IGHV未突变)患者的PFS。完全缓解(CR/CRI)率随伊布替尼治疗时间延长而持续改善,从最初的11%升高至27%。另外,伊布替尼较苯丁酸氮芥更能改善患者的血液学事件如贫血和血小板减少。该研究中,不良反应所致的剂量减少或治疗中断非常少见。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#RESONATE-2#
36
#随访结果#
27
#CLL研究#
32
#Nat#
31
#伊布替尼#
44
#ESO#
30
#重磅#
45