日常吃点抗氧化剂强身健体?强的更可能是癌细胞的体!
2022-01-02 LILYMED MedSci原创
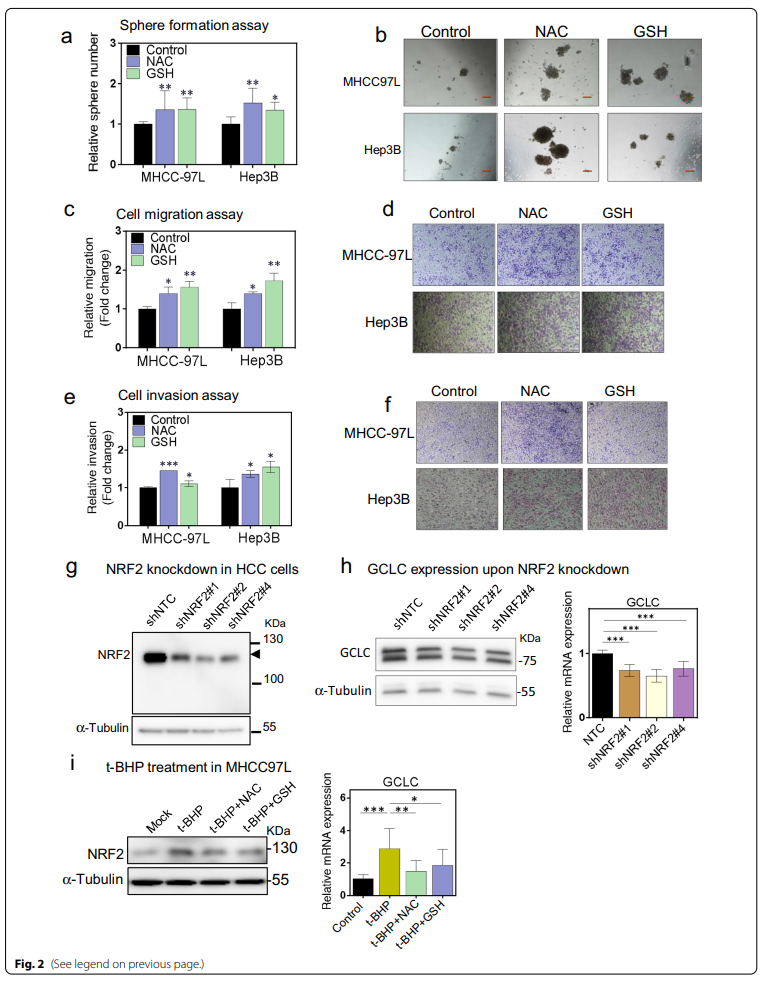
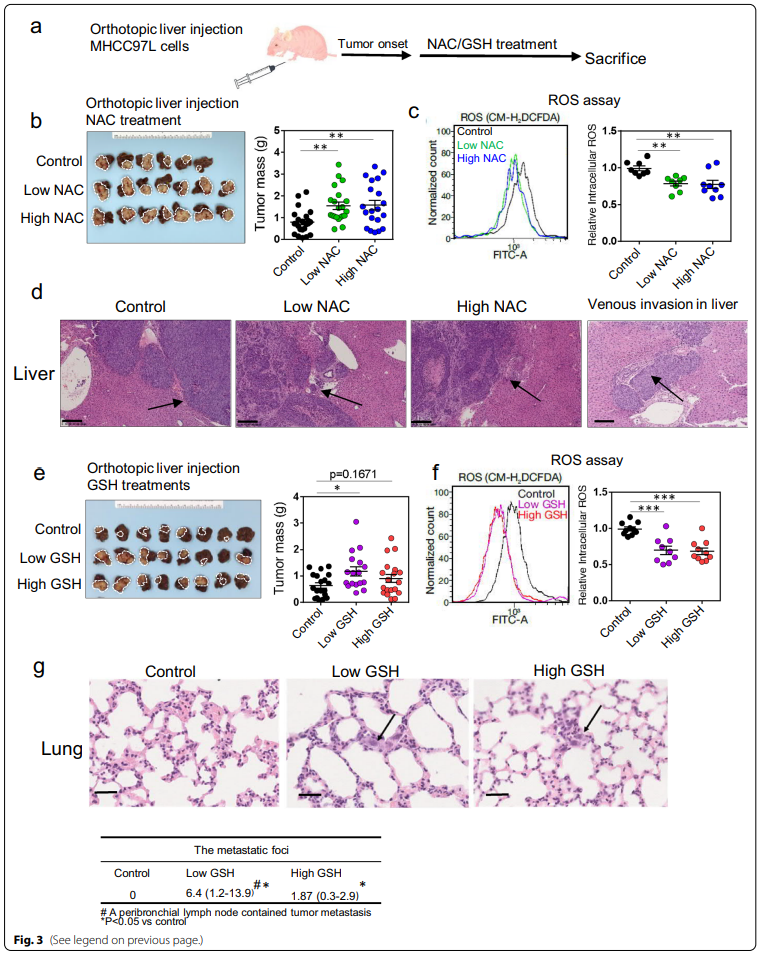
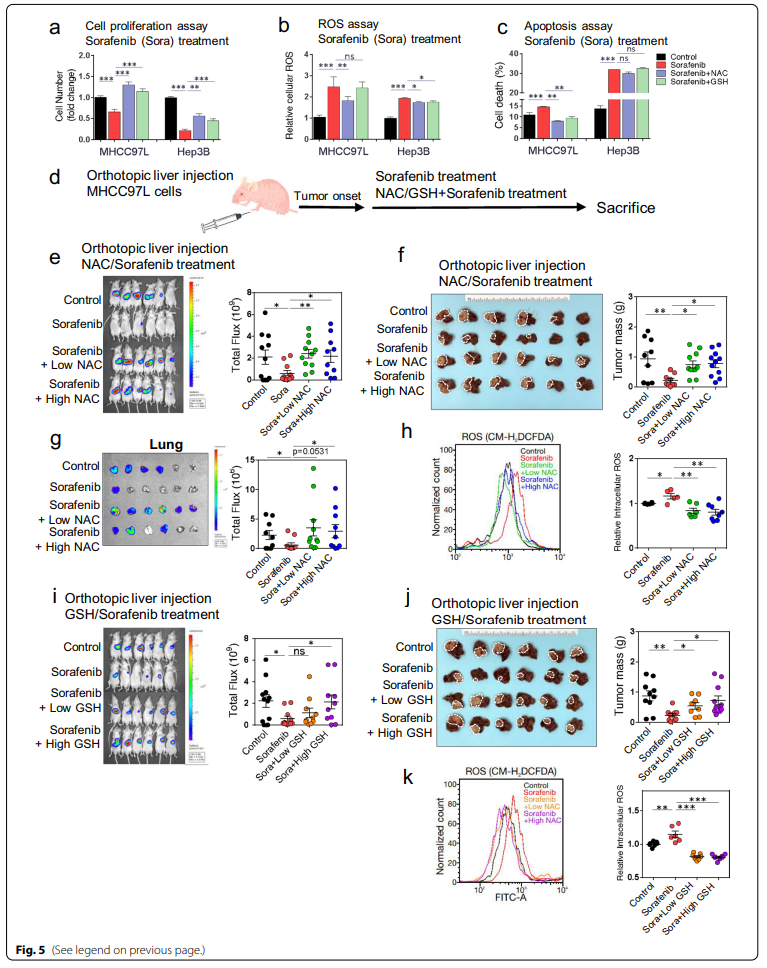
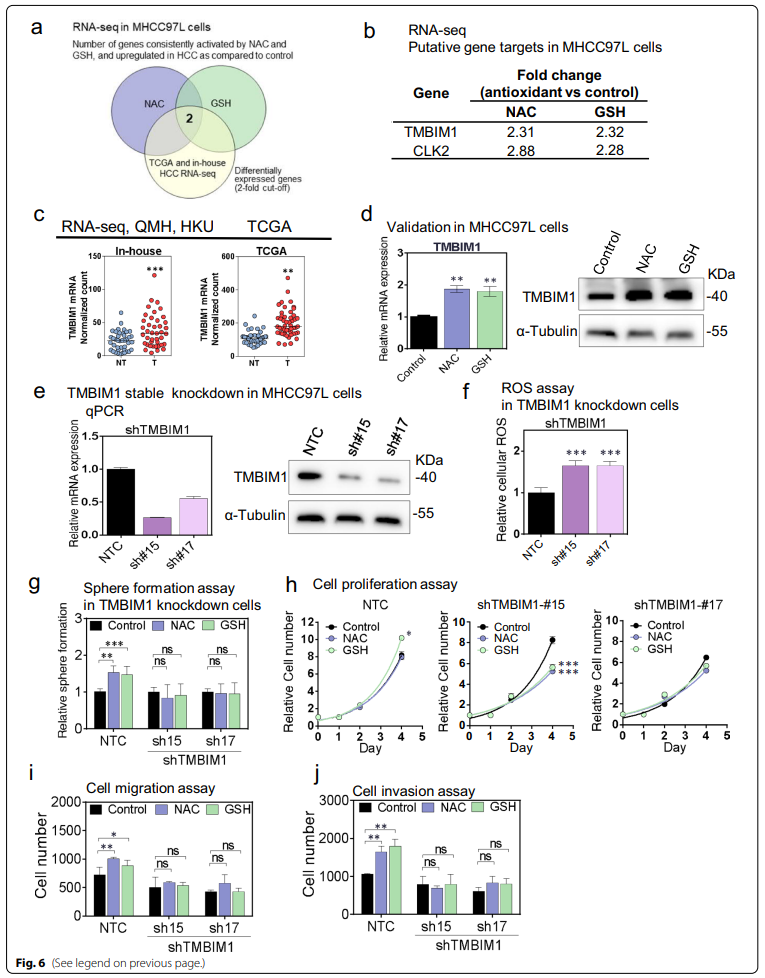
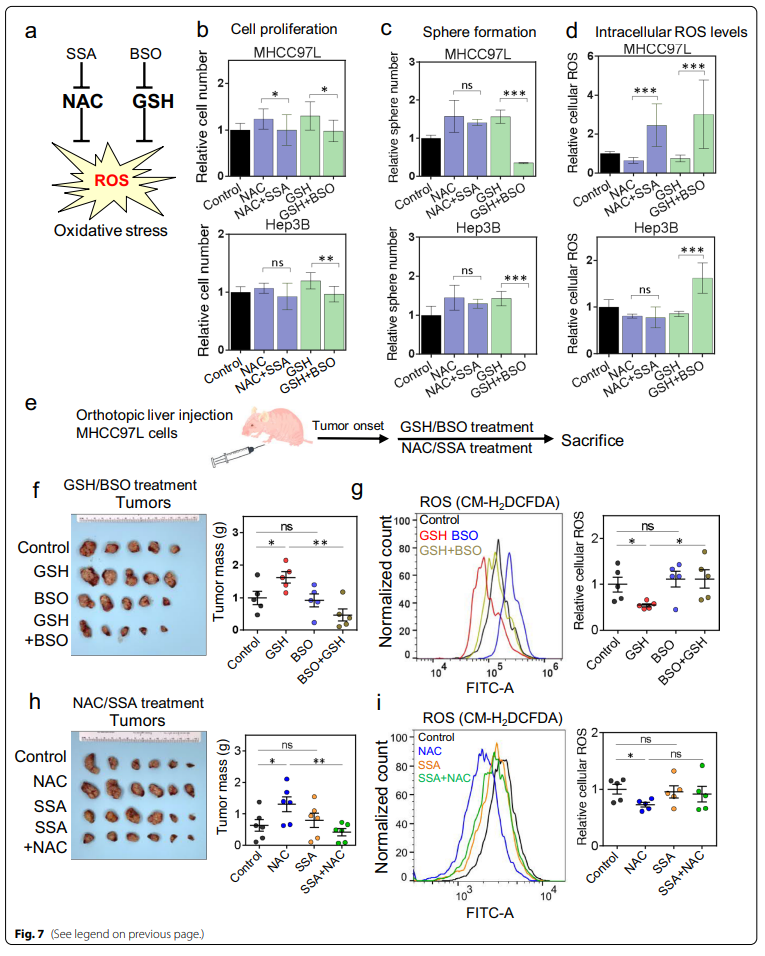
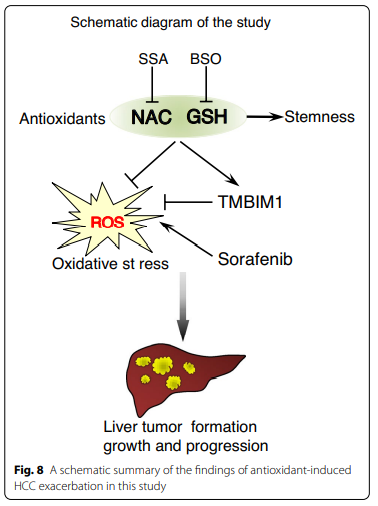
Cell & Bioscience:抗氧化剂补充剂通过降低细胞内ROS和TMBIM1的诱导,促进肝癌的形成和生长,并使肝癌产生耐药性







原文来源:
Zhang et al. Antioxidant supplements promote tumor formation and growth and confer drug resistance in hepatocellular carcinoma by reducing intracellular ROS and induction of TMBIM. Cell & Bioscience (2021) 11:217
https://doi.org/10.1186/s13578-021-00731-0
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#氧化剂#
0
这逼的观点,奇怪的很奇怪的很
68
学习
72
学习了
0
顶级期刊就是好,遗憾接触晚了,我把维生素C和e放了下来。
70
别嘌呤醇是一种著名的黄嘌呤氧化酶抑制剂
63
不错,学习了。
31
#癌细胞#
40
#抗氧化剂#
44