Pediatrics:新冠肺炎疫情期间儿科急诊科脓毒症筛查工具的准确性
2022-05-07 从医路漫漫 MedSci原创
幸存败血症运动建议对急性不适的儿童(如儿科急诊(ed)的儿童)进行败血症和相关疾病的筛查。
背景: 败血症是儿童发病率和死亡率的重要原因。通过早期识别败血症并及时采取适当的治疗措施,可以降低这种发病率和死亡率。幸存败血症运动建议对急性不适的儿童(如儿科急诊(ed)的儿童)进行败血症和相关疾病的筛查。为了便于对败血症进行系统筛查,许多儿科急诊依赖自动筛查工具。之前在儿科急诊环境中对基于全身炎症反应综合征(SIRS)标准的自动化脓毒症算法进行的比较表明,与人工脓毒症筛查相比,该算法在确定脓毒症时具有更高的灵敏度和特异性。自动化脓毒症筛查现已被许多儿科急诊采纳为护理标准。
尽管自动化脓毒症警报提供了许多优于手动警报的优势,但当引入自动化脓毒症警报时,临床医生可能会遭受“警报疲劳”。当警报频繁触发时,尤其是当警报具有低阳性预测值时,会发生警报疲劳。 临床医生对警报变得不敏感。许多成人急诊室最近报告了败血症模型的过度警报,原因是继发于新冠肺炎大流行的医院患者特征的变化。这表明,在新冠肺炎疫情之前训练并部署在成人急诊室的败血症模型可能在新冠肺炎疫情期间表现不佳,并可能导致警报疲劳。 新冠肺炎疫情对儿童和成人患者的影响不同,新冠肺炎对儿童脓毒症警报的影响尚未研究。
目的:本研究的目的是评估儿科急诊中新冠肺炎患者的涌入是否改变了脓毒症警报的频率,或者这些警报在识别低血压感染性休克患者中的表现。了解新冠肺炎疫情期间发出脓毒症警报的频率非常重要,以防止警报疲劳和漏诊脓毒症病例的潜在可避免发病率和死亡率。此外,了解疫情期间脓毒症警报的表现可以使我们进一步优化我们的脓毒症算法,以更好地识别脓毒症患者和非脓毒症患者。
方法:我们对疫情前的59,335名急诊患者和疫情期间的51,990名急诊患者进行了回顾性队列研究,这些急诊患者均有基于全身炎症反应综合征标准的自动脓毒症警报。在疫情之前和疫情阶段之间,以及在疫情阶段新冠肺炎阴性和阳性患者之间,比较了脓毒症算法的敏感性、特异性、阴性预测值和阳性预测值。
结果:在疫情之前,急诊就诊触发脓毒症警报的比例为7.0% (n=4,180),在此期间为6.1% (n=3,199)。在这两个时间段内,每例确诊低血压性脓毒性休克病例触发的脓毒症警报数量均为24。在这些时间段之间,脓毒症警报的敏感性(74.1%对72.5%)、特异性(93.2%对94.0%)、阳性预测值(4.1%对4.1%)或阴性预测值(99.9%对99.9%)没有差异。对于新冠肺炎阳性和阴性患者,警报的敏感性(60%对73.3%)和特异性(87.3%对94.2%)较低。
表1A在COVID-19疫情之前和期间脓毒症筛查算法性能的比较
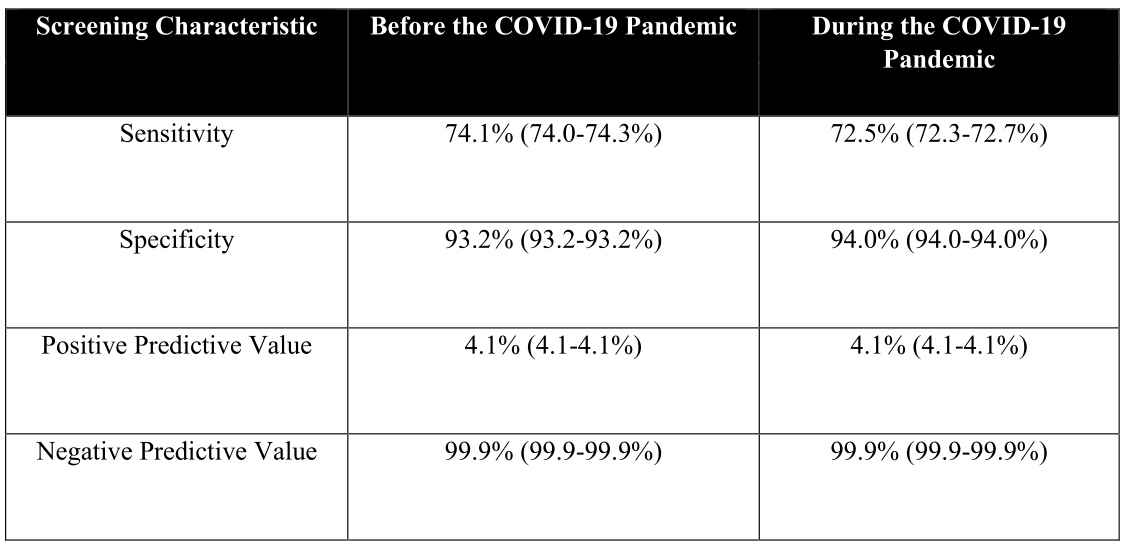
表1B比较新冠肺炎阳性和阴性患者在新冠肺炎疫情期间的脓毒症筛查算法性能
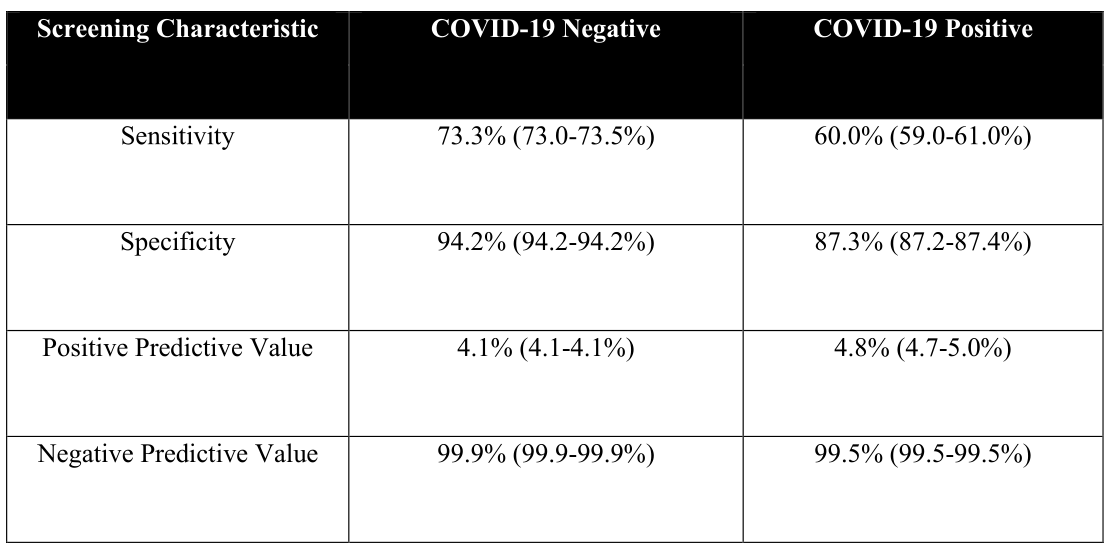
表2在新冠肺炎阳性患者的各种发生率下脓毒症筛选算法性能的模拟

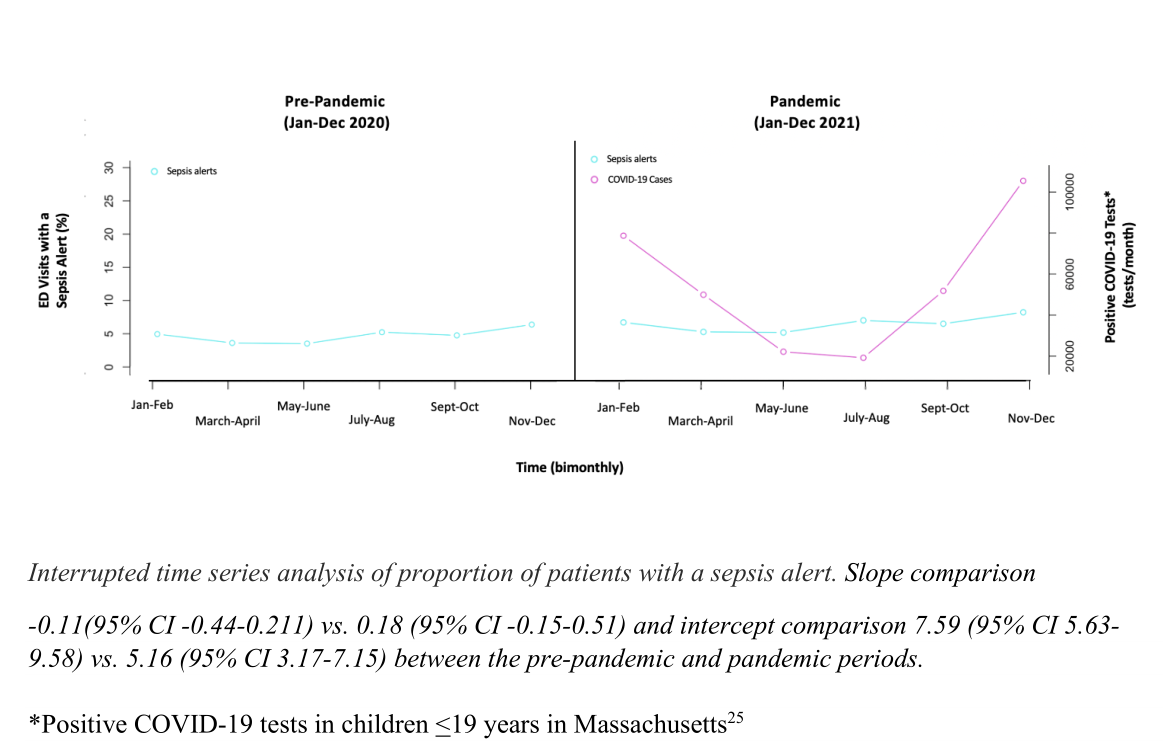
图1急诊脓毒症筛查阳性患者比例的中断时间序列分析
结论:在这项研究中评估的脓毒症警报算法没有导致过多的通知,并在儿科急诊新冠肺炎疫情期间保持了足够的性能。
原文出处:Yan AP, Zipursky AR, Capraro A,et al.Pediatric Emergency Department Sepsis Screening Tool Accuracy During the COVID-19 Pandemic.Pediatrics 2022 May 03
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#DIA#
36
#筛查工具#
42
#PE#
30
#Pediatric#
47
#准确性#
47
#急诊科#
46