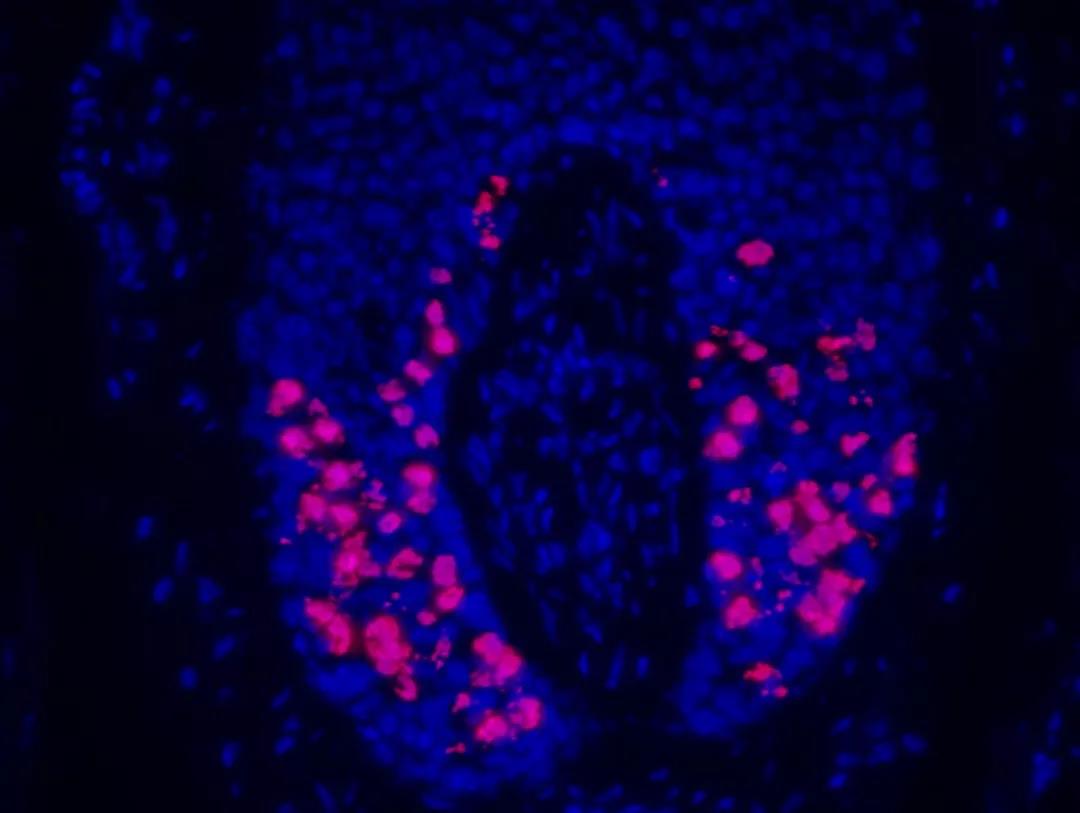
EMBO Mol Med:化疗脱发?靶向药CDK4/6抑制剂或将带来防脱发新突破
2019-09-25 纪艳青 生物探索
脱发是癌症治疗中化疗带来的常见副作用之一,并且在化疗结束后的很长一段时间内都难以恢复。据统计,有高达8%的患者由于担心化疗后脱发而拒绝化疗!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#CDK4#
28
#抑制剂#
25
#新突破#
34
#CDK#
34
#CDK4/6#
23
#Med#
31