iScience:换一个肠道菌群有多难?戴磊团队揭示移植肠道菌群的建立和恢复力
2022-01-22 “生物世界”公众号 “生物世界”公众号
本研究对老龄小鼠进行了来自自体或异体宿主的粪便菌群移植,跟踪观察发现移植后肠道菌群成功定植并分别建立与宿主类似的稳态菌群结构,并对宿主结肠转录组产生长期影响。
2022年1月21日,中国科学院深圳先进技术研究院合成生物学研究所、深圳合成生物学创新研究院戴磊课题组在 Cell 子刊 iScience 杂志发表了题为:Establishment and resilience of transplanted gut microbiota in aged mice(老龄小鼠移植肠道菌群的建立和恢复力)的研究论文。
该研究对老龄小鼠进行了来自自体或异体宿主的粪便菌群移植,跟踪观察发现移植后肠道菌群成功定植并分别建立与宿主类似的稳态菌群结构,并对宿主结肠转录组产生长期影响。此外,对于移植后的小鼠进行化学诱导肠道炎症,发现异体移植建立的菌群经过再次扰动后,无法维持与供体相似的稳态,而是恢复为老龄宿主移植前的初始状态。本研究说明对于老龄宿主进行异体肠道菌群移植后应该长期关注其稳定性并在有需要时进行重复移植。
助理研究员王莹博士、中国科学院大学硕士生汤锦辉为共同第一作者,戴磊研究员为通讯作者。共同作者包括中国科学院深圳先进技术研究院脑认知与脑疾病研究所的刘欣安副研究员、王立平研究员,哈佛大学医学院的刘洋彧教授,深圳未知君生物科技的谭验博士等人。
肠道菌群与宿主共生,在长期地相互作用下建立起了高度适配的状态,具有很强的稳定性。维持健康的肠道菌群对老年人的生活质量和健康寿命至关重要,许多胃肠道疾病,包括艰难梭菌感染(CDI),炎症性肠病(IBD)和肠易激综合症等均与菌群失调有关,而且其中许多疾病在老年人中更为普遍。
粪便菌群移植(FMT)是一种将粪便物质从健康供体转移到肠道菌群受到破坏的患者的手段,目前已被用于治疗多种疾病。评估FMT治疗的成功和保护效果的两项重要指标,分别是:
1)是否能在宿主体内建立新的菌群稳态;
2)新建立的菌群稳态在再次扰动后是否仍具有恢复能力。
尤其是在异体FMT的情况下,原本与宿主高度适配的菌群状态被来自供体的具有不同组成的新状态所取代,它可能处于亚稳态,这种新建立的菌群平衡可能更容易被环境变化所破坏,因此研究移植后菌群的稳定性和恢复力至关重要。
粪便菌群移植(Fecal Microbiota Transplantation)示意图(修改自2019, Wang, J Formos Med Assoc)
老年人作为胃肠道疾病高发人群,是否可以受益于FMT治疗呢?此前有研究表明 FMT 在治疗老年患者的 CDI 方面是安全有效的,但在 FMT 后的 6 个月内,老年患者的复发率显着高于年轻患者。一项以小鼠为模式动物的研究比较了幼年(3 周龄)和成年(8 周龄)小鼠FMT后菌群的长期状态,发现菌群定植在幼年 SPF 小鼠中优于成年 SPF 小鼠,这表明移植菌群的建立可能受到宿主年龄的影响。
目前尚无对自体与异体FMT后移植菌群在老年宿主中的长期稳定性和恢复力的相关研究。如何合理设计在老年宿主中使用 FMT 的治疗策略?是否需要采取特定的预防措施防止疾病复发?本项研究使用老龄小鼠模型对此进行探究。
研究人员使用自然衰老的小鼠(20月龄)作为FMT受体来研究移植的肠道菌群的建立及其恢复力。首先,用抗生素混合物处理老龄小鼠以破坏肠道菌群,并监测其自行恢复(spontaneous recovery, SR)过程。研究发现,抗生素处理对肠道菌群多样性和组成的影响持续至处理后 8 周。
接下来,研究人员对抗生素处理后的老龄小鼠进行自体(Autologous, FMT-A)或异体(Heterologous,FMT-H)的FMT,比较他们对于促进肠道菌群稳态恢复的作用(图1A)。异体移植的供体是来自另一供应商的2月龄年轻小鼠,它们的初始肠道菌群与老龄受体的组成显着不同。我们的研究发现与自行恢复(SR)组相比,自体和异体FMT均能将肠道菌群多样性的恢复时间从8周加快到3周(图1B,C)。在抗生素处理后第21天,自体和异体菌群移植分别成功地在新宿主中建立起了新的菌群状态,并且起组成分别接近于供体的菌群组成(图1D-F)。此结果表明在移植菌群的建立层面,异体与自体菌群移植一样有效,并且新建立的菌群组成相似于供体。
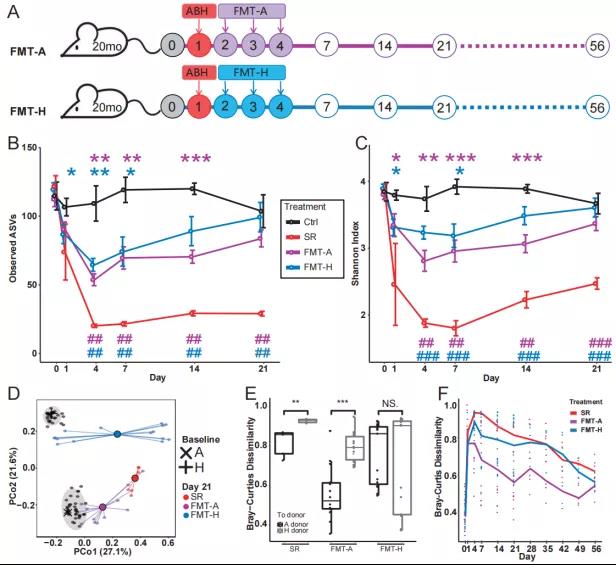
图1:自体或异体FMT均可促进老龄小鼠抗生素处理后的肠道菌群建立
FMT可能引起肠道菌群功能基因的组成(由宏基因组测序表征)和宿主肠道基因表达水平(由结肠转录组测序表征)的重大变化,并影响FMT治疗的成功与否。研究人员跟踪观察了老龄小鼠的三个治疗组(SR,FMT-A和FMT-H)从治疗前到粪菌移植后56天的宏基因组和结肠转录组变化,发现相比于SR和FMT-H组,FMT-A促进微生物群功能恢复方面效果较好。结肠转录组测序则表明,与 SR 组相比,异体和自体FMT均可促进宿主转录组的恢复,而且FMT及不同的供体选择对于宿主转录组具有长期的影响。
最后,研究人员对接受自体或异体FMT后的小鼠使用化学物质(葡聚糖硫酸钠,DSS)诱发结肠炎症,引起对新建立的肠道菌群稳态的再次扰动(图2A)。对于接受自体移植的老龄小鼠,肠道菌群的恢复过程仅被诱导的炎症短暂地扰动,第 53 天后的无论是诱发肠炎的受体鼠(FMT-A-DSS组)还是移植后没有诱发肠炎的受体鼠(FMT-A组)其肠道菌群组成均相似(图 2B),与老年供体的距离没有显着差异(图 2D)。相反,异体移植所建立的肠道菌群则无法在扰动后维持其组成,异体移植后接受肠炎诱导的小鼠(FMT-H-DSS)其菌群组成逐渐恢复到了移植前老龄小鼠原始的菌群稳态(图2C),与仅接受异体粪菌移植(FMT-H组)小鼠相比其菌群组成明显偏离其供体(图 2D)。
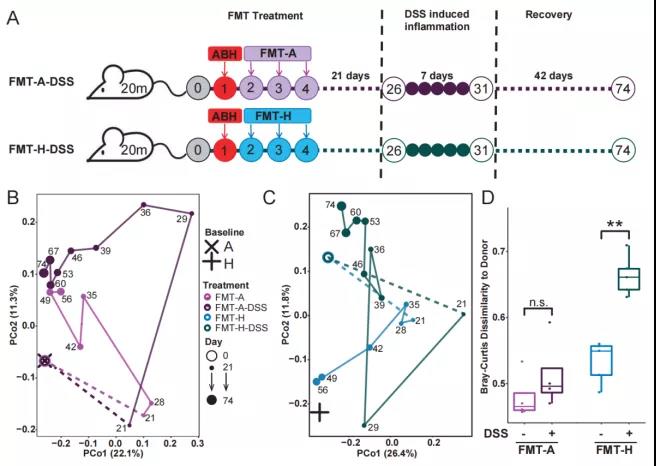
图2:相比于自体FMT,异体FMT后建立的移植菌群在再次扰动后恢复力较差
本项研究表明,异体FMT作为临床上广泛使用的肠道菌群干预手段,不仅应该关注其安全性和有效性,也有必要关注其长期的稳定性。尽管 FMT 已成为复发性 CDI 的最有效治疗方法,但据报道,约 20% 的患者在初始 FMT 治疗后仍会出现复发性 CDI。先前对 IBD 患者进行 FMT 治疗的研究也表明,需要多次 FMT 干预才能获得更好的临床结果,并且有研究显示供体和患者之间的年龄差异显着影响 FMT 后的长期维持。
本研究发现供体的选择不仅对 FMT 后肠道菌群的宏基因组和宿主的转录组有长期影响,也决定了移植菌群应对后续再次扰动的恢复能力。总之,对于老年患者,尤其是接收异体粪菌移植的老年患者,监测 FMT 的长期稳定性和后续扰动(如疾病复发)对于新建立菌群稳态的影响至关重要,在复杂的扰动的情况下可能需要进行多次 FMT或制定更合理的治疗策略。
原始出处:
Ying Wang, et al. Establishment and resilience of transplanted gut microbiota in aged mice. iScience, December 17, 2021. DOI:https://doi.org/10.1016/j.isci.2021.103654.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












学习!
49
学习
54
#SCIE#
38
#肠道菌#
46
#ISC#
36
学习
68
学习学习学习
68