JAMA Network Open:中国研究发现哺乳时间长的妈妈脑卒中风险低
2022-03-04 影像小生 MedSci原创
哺乳与卒中风险的降低显著相关,特别是缺血性卒中,这强调了促进母乳喂养作为卒中有针对性的预防策略的重要性。
以前的大多数研究都集中在哺乳期和心血管疾病之间的联系。然而,很少有研究探讨哺乳与中风亚型之间的关系。美国的一项研究表明,哺乳期较长与中风风险较低相关,但哺乳期与中风不同病理亚型(如缺血性中风、脑出血和蛛网膜下腔出血)的关系并未得到评估。
为了填补这一知识空白,Ziyang Ren等在JAMA Network Open杂志发表研究文章Lactation Duration and the Risk of Subtypes of Stroke Among Parous Postmenopausal Women From the China Kadoorie Biobank, 探讨哺乳期长短与绝经后妇女脑卒中及其亚型的关系。

这项基于人群的前瞻性队列研究研究对象为中国45-79岁的绝经后经产妇(2004-2008年)。在随访期间(2008-2015年),通过疾病登记和国家健康保险索赔数据库评估了新发卒中及其亚型(缺血性卒中、脑出血[ICH]和蛛网膜下腔出血[SAH])。
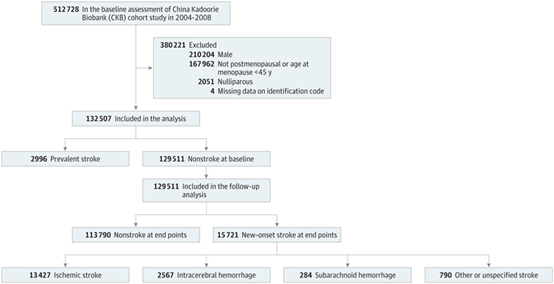
该实验的主要结果和指标为全脑卒中、缺血性卒中、脑出血和蛛网膜下腔出血。该研究采用多变量Cox回归计算卒中和各亚型的调整危险比(aHRs)。129511例绝经后经产妇(中位[IQR]年龄,58.3[54.0-64.6]岁)基线时无卒中,15721例发生卒中,13427例缺血性卒中妇女的中位(IQR)哺乳时间为42.0(24.0-70.0)个月,2567例脑出血妇女的中位(IQR)哺乳时间为54.0(36.0-84.0)个月,284例SAH患者中36.0(24.0-64.5)个月。
与从未哺乳过的绝经后妇女相比,哺乳期至少7个月的妇女发生缺血性中风(aHRs范围为0.52 ~ 0.64)和脑出血(aHRs范围为0.56 ~ 0.78)的风险较低。
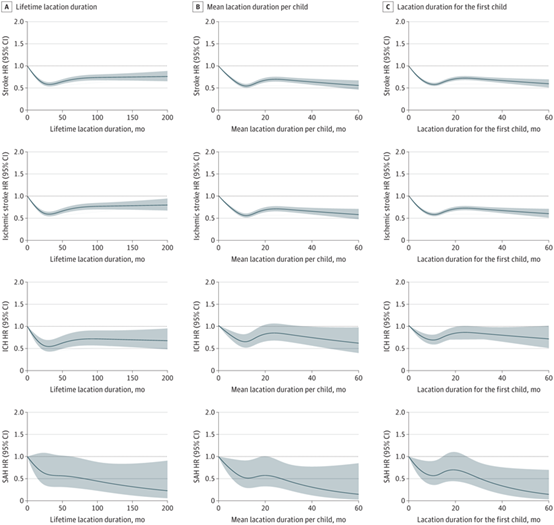
绝经后妇女哺乳期长短与卒中及其亚型的剂量-风险关系。根据年龄、妊娠率、绝经年龄、活产数、糖尿病、高血压、癌症、服用避孕药、抗凝治疗、降血脂治疗、教育程度、收入、婚姻状况、职业、居住地、吸烟、被动吸烟、饮酒、代谢当量、体重指数和腰围调整HRs。
然而,对于SAH,这种关联仅在终生哺乳时间超过24个月的参与者中被发现(aHR, 0.61 [95% CI, 0.47-0.79])。此外,平均每个孩子哺乳时间或第一个孩子哺乳时间为7个月以上的妇女不太可能患中风(aHRs:0.53-0.65)及其亚型(aHRs:0.51-0.75)。
在这项队列研究中,哺乳与卒中风险的降低显著相关,特别是缺血性卒中,这强调了促进母乳喂养作为卒中有针对性的预防策略的重要性。
原文出处
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#研究发现#
46
#PE#
28
#NET#
19
#卒中风险#
35
#哺乳#
36