JNNP:接受奥克列珠单抗治疗的多发性硬化症患者对SARS-CoV-2疫苗的免疫应答与外周免疫细胞谱的关系
2022-03-02 MedSci原创 MedSci原创
冠状病毒疾病是由SARS COV-2引起的一种高度传染性疾病。SARS-CoV-2的迅速传播导致了全球大流行,对人们的个人生活、医疗保健系统和经济产生了负面影响。冠状病毒疾病疫苗接种是一种有希望的降低
冠状病毒疾病是由SARS COV-2引起的一种高度传染性疾病。SARS-CoV-2的迅速传播导致了全球大流行,对人们的个人生活、医疗保健系统和经济产生了负面影响。冠状病毒疾病疫苗接种是一种有希望的降低COVID-19发病率和死亡率的方法,有可能抑制全球流感大流行。冠状病毒疾病疫苗在临床试验中显示出了高的疗效,在预防COVID-19传播和严重疾病的过程中,疫苗在2020年底开始上市。 冠状病毒疾病疫苗抗原的靶抗原是SARS COV-2的抗原(S)蛋白,其结合宿主细胞介导的病毒融合的ACE 受体。目前,可以使用不同的疫苗方法,包括mRNA、复制不全载体、重组蛋白和灭活疫苗。肌肉注射一剂或两剂疫苗,并引发B细胞反应,从而产生结合中和抗体(abs)和T细胞反应。冠状病毒疾病疫苗的安全性和有效性的临床试验仅包括免疫活性人群,而不包括接受免疫调节治疗的患者。Ocrelizumab(OCR)是一种靶向CD20的选择性单克隆抗体,被批准为复发缓解型和原发性进行性多发性硬化症(RRMS和PPMS)的疾病调节疗法(DMT)。 200多个 全球已有1000名患者接受了OCR治疗。机制上,OCR通过补体介导的细胞溶解、细胞介导的吞噬和细胞毒性选择性地消耗CD20表达细胞。虽然大多数B细胞表达CD20,但只有3%-5%的T细胞表达CD20。
B细胞是适应性免疫反应的一个重要组成部分,为抵抗病原体提供保护。通过产生各种细胞因子,它们塑造并促进T细胞反应,促进淋巴组织的形成。此外,通过终末分化为浆细胞,它们是产生抗原特异性免疫球蛋白的来源。因此,之前的研究报告,接受B细胞调节疗法的患者接种疫苗后体液免疫反应减弱。然而,特别是对于这些患者,对疫苗接种的充分免疫反应非常重要,因为他们可能会增加感染、严重病程和病毒进化的风险。冠状病毒疾病或疫苗接种后,尽管B细胞应答减弱,但似乎保留了SARS COV-2抗原特异性T细胞应答。这些结果与T细胞上CD20的低表达水平一致。然而2019冠状病毒疾病的体液免疫应答与临床参数和外周免疫细胞谱的关系研究在多发性硬化症(MS)接受OCR的患者中是罕见的。此外,外周B细胞区的差异及其对SARS-CoV-2特异性免疫反应的影响之前尚未研究过。在本文,59例冠状病毒疾病患者的外周血B细胞分布和临床特征进检查,分析了体液和T细胞介导的免疫应答。本文发表在《神经病学,神经外科学和精神病学杂志》上().
进行了一项回顾性研究,包括59名接受OCR治疗的MS患者,他们接受了SARS-CoV-2疫苗接种。抗SARS-CoV-2抗体滴度、血常规参数和外周免疫细胞谱在第一次(基线)之前测量,中位数为4 第二次接种疫苗数周后(随访)。此外,在随访中还分析了SARS-CoV-2特异性T细胞反应和外周血B细胞亚群。最后,评估与疫苗接种相关的不良事件。在临床常规检查期间采集血样。用SepMate分离管(StemCell Technologies)通过Ficoll梯度从全血中分离外周血单个核细胞(PBMC),并在液氮中冷冻保存。对于FC,将PBMC解冻并重新悬浮在FC缓冲液(磷酸盐缓冲盐水(PBS)/牛血清白蛋白(BSA)/EDTA)中。样品离心5分钟 1500分钟 转速和4°C时,丢弃上清液。加入FC缓冲液,将细胞转移到96孔板上。重复离心,将细胞重新悬浮在含有FcR阻断试剂(Miltenyi Biotec)的FC缓冲液中。在第二次2019冠状病毒疾病疫苗接种后4周内,用SARS COV-2干扰素γ释放试验(IGRA,EUROIMUN)评估SARS COV-2对T细胞的反应。根据制造商的说明,使用SARS-CoV-2-IGRA刺激试剂盒(Euroimmun)制备血样。

奥雷利珠单抗治疗的长期疗效
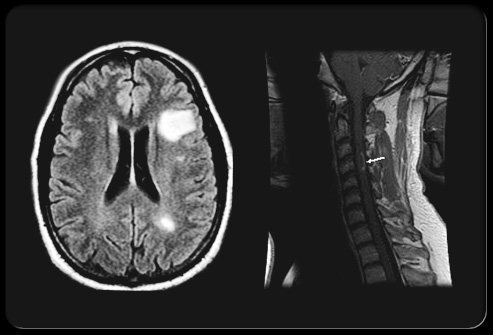
接种疫苗后,我们在27.1%的MS病例中发现了抗SARS-CoV-2(S)抗体,在92.7%的MS病例中发现了SARS-CoV-2特异性T细胞应答。在没有抗SARS-CoV-2(S)抗体的患者中,T细胞介导的干扰素(IFN)-γ释放更为明显。抗体滴度与外周血B细胞计数、上次输注后的时间和总IgM水平呈正相关。它们与之前的输液周期数呈负相关。抗体阳性患者外周血浆细胞增多。T细胞反应与外周血淋巴细胞计数呈正相关。此外,IFN-γ释放与上次输注后的时间呈负相关。

接受奥克列珠单抗的MS患者对SARS-CoV-2疫苗的保留T细胞反应
冠状病毒疾病的临床试验表明,COVID-19疫苗在预防病毒传播和严重疾病方面具有很高的疗效。然而,免疫功能低下的患者,可能会增加感染风险,16-20名患者已被排除在这些试验之外。评估接受OCR的MS患者感染风险的研究得出了相反的结果。虽然一些人报告冠状病毒疾病易感性增加,但不能将治疗与B细胞衰竭疗法联系在一起,从而提高感染率。冠状病毒疾病的研究表明,接受B细胞调节疗法的患者在COVID-19疫苗接种中体液免疫应答减弱,而T细胞应答似乎得以保留。在接受OCR的59名MS患者中评估了抗SARS-CoV-2-abs,在27.1%的患者中只能检测到阳性的抗SARS-CoV-2-abs。相比之下,在其他DMT(例如芬戈利莫德85.7%,IFN-β96.4%和克拉屈滨100%)的大多数MS患者中,先前发现了抗SARS-CoV-2-ab反应。正如预期的那样,抗SARS-CoV-2(S)-abs与OCR治疗的MS患者外周血B细胞数量相关。这与之前在接受B细胞调节治疗的患者中观察到的结果一致。
接受OCR的MS患者可以对SARS-CoV-2疫苗接种产生足够的T细胞免疫应答,而抗SARS-CoV-2(S)-abs的产生似乎受到影响。因此,测量T细胞效应器机制可能适合于评估免疫功能低下患者的疫苗反应。鉴于OCR的长期和异质性效应,监测外周血B细胞可促进个体化治疗方案,并可能成为确定最佳接种时间的工具。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言


















#多发性#
34
#硬化症#
41
#SARS-CoV#
36
新颖的研究方向……
46
#SARS#
35
#免疫应答#
0