JAMA:无症状严重颈动脉狭窄患者的缺血性中风发生率有多高?
2022-06-06 MedSci原创 MedSci原创
无症状严重颈动脉狭窄患者队列中,没有进行手术干预,同侧颈动脉相关急性缺血性卒中的估计比率在5年内为4.7%。
由于医疗技术的进步和缺乏比较医疗和手术治疗的当代数据,无症状重度颈动脉狭窄患者的最佳治疗方法尚不确定。为此,来自美国加利佛尼亚大学的专家开展了相关研究,旨在估计经药物治疗的无症状严重颈动脉狭窄患者的卒中结局。
研究者开展了一项回顾性队列研究,包括3737名在2008年至2012年期间诊断为无症状重度(70%-99%)颈动脉狭窄的成年参与者,在之前的6个月内没有进行干预或同侧神经系统事件。参与者接受随访至2019年,所有参与者都是为450万会员服务的美国综合区域卫生系统的成员。
主要的暴露因素为影像诊断为无症状的颈动脉狭窄70%-99%患者。主要结局为同侧颈动脉相关急性缺血性卒中的发生率。
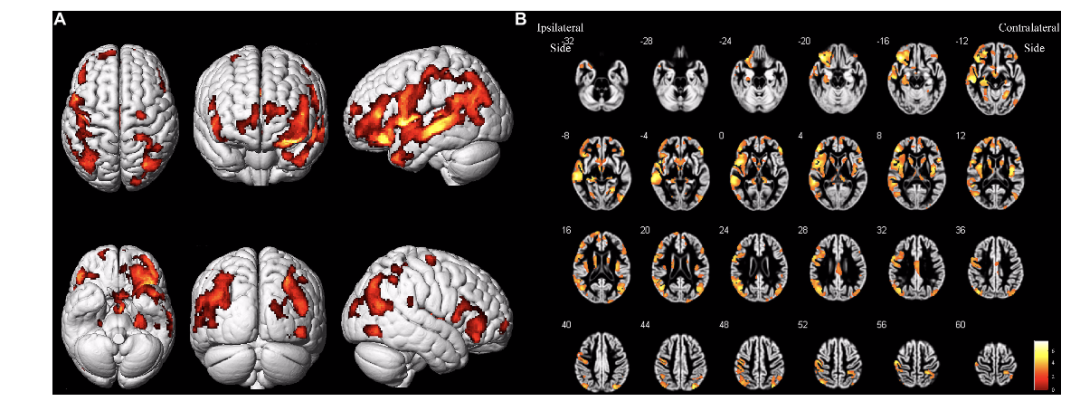
在94 822名有合格影像学研究的患者中,3737名(平均年龄73.8岁[SD 9.5岁];57.4%为男性)患者的4230条动脉符合选择标准,包括2314名从未接受干预的患者。该队列的平均随访时间为4.1年(SD 3.6年)。
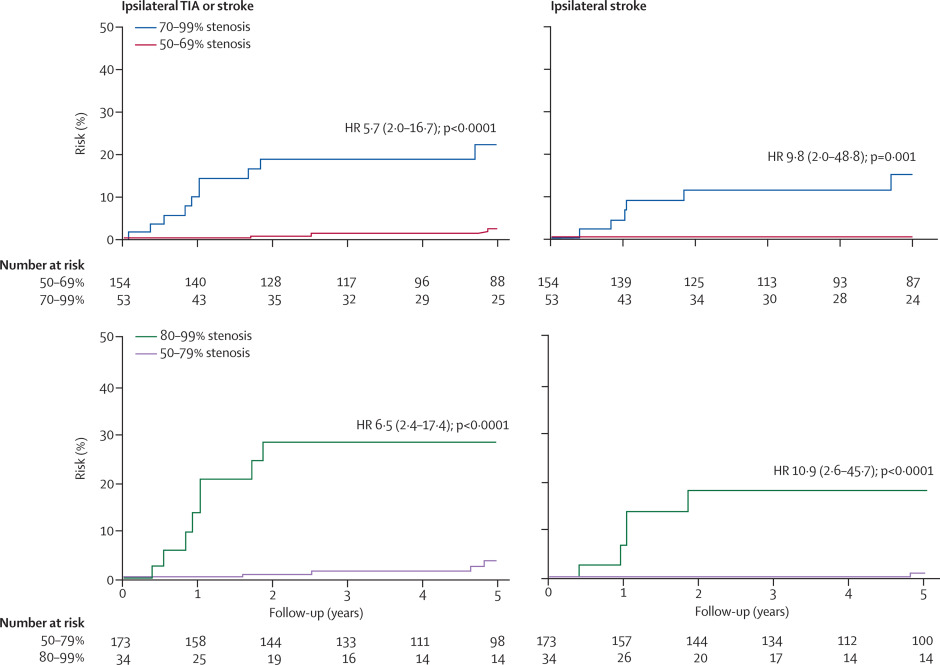
在接受任何手术干预之前,共有129名患者发生133例狭窄颈动脉的同侧缺血性中风事件。从研究开始到发生中风事件的中位时间为24.8(IQR 7.9-46.5)个月。平均年发生率为0.9%(95%CI,0.7%-1.2%),经Kaplan-Meier生存分析估算,5年同侧缺血性中风的发生率为4.7%(95%CI,3.9%-5.7%)。
综上,在一个以社区为基础的无症状严重颈动脉狭窄患者队列中,没有进行手术干预,同侧颈动脉相关急性缺血性卒中的估计比率在5年内为4.7%。
参考文献:
Incidence of Ischemic Stroke in Patients With Asymptomatic Severe Carotid Stenosis Without Surgical Intervention. JAMA. 2022;327(20):1974–1982. doi:10.1001/jama.2022.4835
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#发生率#
66
#颈动脉#
54
#缺血性#
41
#无症状#
43
#动脉狭窄#
42
#缺血性中风#
52
看来还是治疗好一些。
48
JAMA上文章都是顶级的,谢谢梅斯及时上新
30