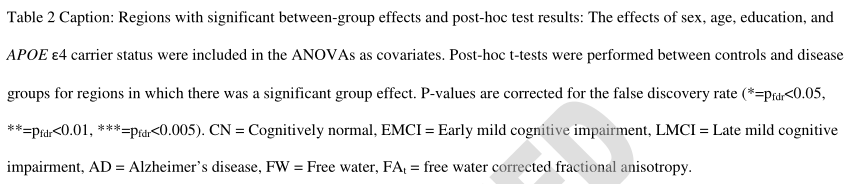
Neurology:认知障碍与 Meynert 基底核和蓝斑核至经内嗅皮层中游离水(FW)的关联
2022-01-08 Naomi MedSci原创
近日,有研究人员通过临床诊断、认知表现、痴呆症严重程度和血浆神经丝轻链浓度评估,确定扩散微结构与阿尔茨海默病(AD)严重程度早期变化的关系。FW是与认知障碍相关的结构改变的非侵入早期生物标志物。
细胞外淀粉样蛋白β聚集体和细胞内tau病变是AD的病理特征。然而,其他神经变性标志物是AD临床症状的有力预测指标。游离水(FW)是一种弥散磁共振成像测量方法,可以估计细胞外间隙的体积分数,通常在神经变性的情况下增加。最近的研究结果表明,与脑萎缩相比,FW可能是神经变性的更有效的早期标志物。然而,目前尚不清楚FW与临床诊断、临床治疗以及血浆神经丝轻链等全局性神经变性的检测之间的关系。
尸检研究表明,AD相关tau病变出现在蓝斑到Meynert基底核、经嗅皮层、内嗅皮层、海马到新皮质。近日,有研究人员通过临床诊断、认知表现、痴呆症严重程度和血浆神经丝轻链浓度评估,确定扩散微结构与阿尔茨海默病(AD)严重程度早期变化的关系。
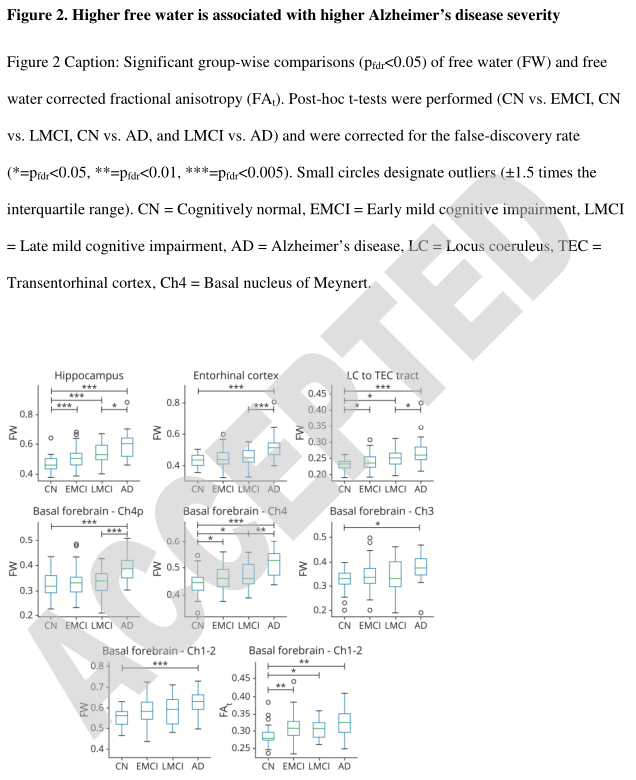
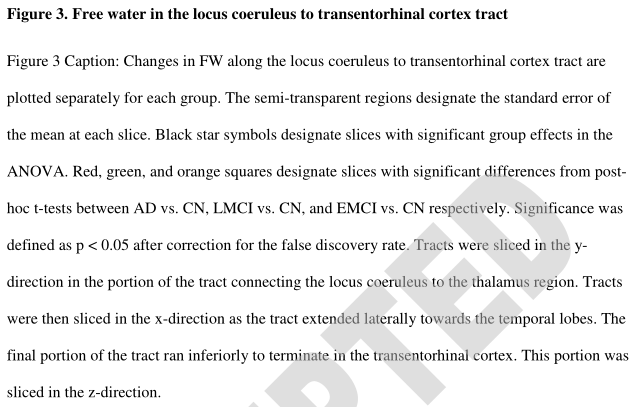
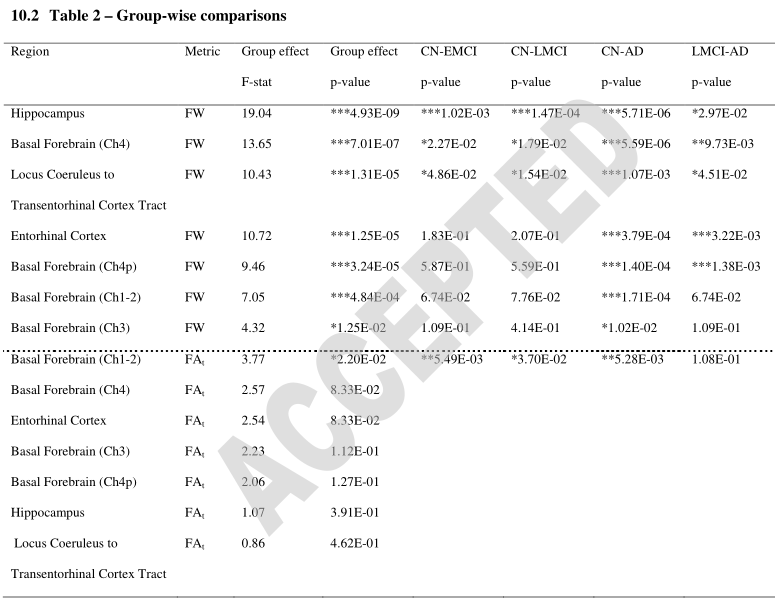
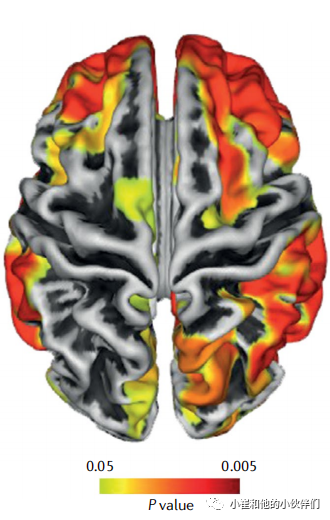
该研究假设,在痴呆严重程度较低的组中,蓝斑到经嗅觉皮质束和Meynert基底核的FW将升高,其他区域只会随着痴呆严重程度的进展而受到影响,并进一步预测FW与临床指标和血浆神经丝轻链浓度相关。对认知正常受试者(CN)、早期轻度认知损害(EMCI)、晚期轻度认知损害(LMCI)和AD患者进行了弥散MRI扫描。计算蓝斑-经嗅觉皮质束、基底前脑四个大细胞区(如Meynert基底核)、内嗅皮层和海马的游离水(FW)和FW校正的分数各向异性(FW)。所有患者都接受了一系列的认知评估,并在血浆样本中测量了神经丝轻链水平。
- 在蓝斑-嗅觉皮质束、Meynert基底核和海马,EMCI组的FW明显高于CN组(平均Cohen d=0.54;pfdr<0.05)。
- AD组的FW明显高于CN组(平均Cohen d=1.41;Pfdr<0.01)。
- 海马、内嗅皮质、Meynert基底核和蓝斑至经嗅皮质束的FW与所有五项认知损害指标和神经丝轻链水平呈正相关(平均R2=0.10;pFDR<0.05)。
结果表明,较高的FW与较严重的临床诊断、认知障碍和神经丝轻链有关。研究还提示,在从CN过渡到EMCI的过程中,蓝斑到经嗅觉皮质束、Meynert基底核和海马的FW升高,而其他基底前脑区和内嗅皮层直到AD后期才受到影响。FW是与认知障碍相关的结构改变的临床相关和非侵入性早期标志物。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#Neurol#
34
#蓝斑核#
36
Good
52
好文章,谢谢分享。
63