Int J Urol:前列腺癌根治性切除术后,患者应该观察多久?
2022-02-08 AlexYang MedSci原创
通过使用Weibull分析方法调查了前列腺特异性抗原失败和其他原因死亡的风险率,从而确定术后观察时间。
PCa是全世界男性中第二大常见癌症。对PCa进行根治性切除的方法有几种,包括耻骨后根治性前列腺切除术、LRP或机器人辅助LRP。然而,目前还没有关于这些干预措施实施后,推荐的观察时间报告。到目前为止,许多研究已经调查了存活率,并确定了观察方法,但无论何种手术方式,都没有建立标准的术后观察期。

近期,来自日本的研究人员在《Int J Urol》上发表文章,由于目前对于接受前列腺癌根治术的患者还没有建议的观察时间,他们通过使用Weibull分析方法调查了前列腺特异性抗原失败和其他原因死亡的风险率,从而确定术后观察时间。
研究纳入了2002年6月至2017年12月期间,接受腹腔镜前列腺癌根治术的612名患者。按D'Amico风险分类,研究人员将患者分为三个年龄组:<60岁,60-69岁和≥70岁。每个时间点的风险率均由Weibull分析得出。腹腔镜前列腺根治术后的最佳观察时间确定为其他原因死亡的风险率超过前列腺特异性抗原失败风险率的交叉点。
研究结果发现,在所有按年龄分类的组别中,其他原因死亡的风险率随着时间的推移而增加。相比之下,前列腺特异性抗原失败的风险率逐渐下降。≥70岁的年龄组显示出最高的风险率。前列腺特异性抗原失败的风险率在高风险组中最高。低风险组中年龄≥70岁和60-69岁的患者分别建议观察6年6个月和14年8个月,其余患者建议进行>25年的术后观察。
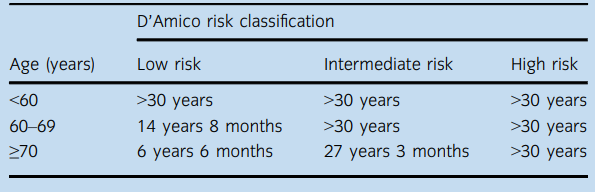
LRP后的最优观察时间
综上所述,腹腔镜前列腺根治术后的观察时间,可以通过比较基于Weibull分析的前列腺特异性抗原失败和其他原因死亡的估计风险率来评估。泌尿外科医生应注意年龄和风险分类,以便进行最佳的术后观察。
原始出处:
Masanori Hasegawa , Koichiro Yamada , Keisuke Shigeta et al. How long should urologists observe patients with prostate cancer after radical prostatectomy? Weibull analysis. Int J Urol. Jan 2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#切除术#
42
很好
47
#根治性切除术#
40
#根治#
55
学习了
46
认真学习了
61
学习了,谢谢分享
52