外泌体(Exosome)知识与检测方法
2015-09-16 MedSci MedSci原创
一、 Exosome 简介 最近几年,一种叫做Exosome的小囊泡正受到大家广泛的关注。Exosome是直径约为30-150nm,密度在1.13-1.21g/m1的小囊泡。Exosome天然存在于体液中,包括血液、唾液、尿液和母乳,外泌体(Exosome)是活细胞分泌的来源于晚期核内体(也称为多囊泡
一、 Exosome 简介
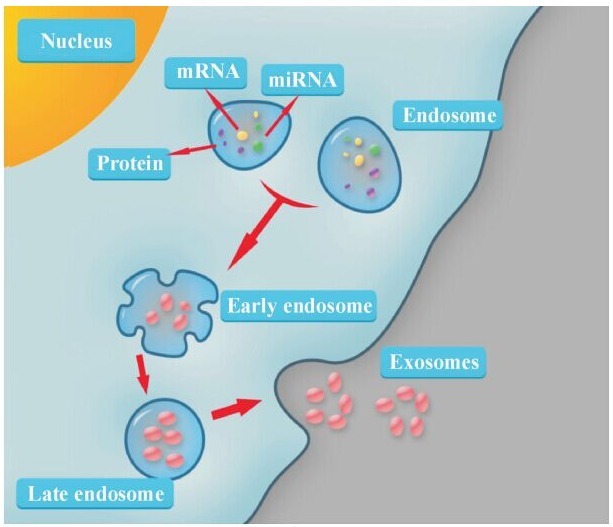
最近几年,一种叫做Exosome的小囊泡正受到大家广泛的关注。Exosome是直径约为30-150nm,密度在1.13-1.21g/m1的小囊泡。Exosome天然存在于体液中,包括血液、唾液、尿液和母乳,外泌体(Exosome)是活细胞分泌的来源于晚期核内体(也称为多囊泡体 )的膜性囊泡。
Exosome在30年前被人们所发现。早期的研究认为,exosome执行蛋白运输功能,特异靶定受体细胞,交换蛋白和脂类或引发下游信号事件。直到2007年,研究人员发现exosome也运输核酸,参与细胞间通讯。总之,其蛋白、RNA和脂肪成分特异,且携带了一些重要的信号分子,有望在多种疾病的早期诊断中发挥作用,这使得exosome的市场也在快速扩展,并成为热门的研究对象。不同组织细胞来源
exosome由于携带的蛋白质不同,而能够发挥不同的生物学功能。例如,肿瘤细胞分泌的exosome能够介导血管再生肿瘤细胞增殖及免疫逃逸;而树突状细胞源性exosome则能够引起机体有效的抗肿瘤免疫应答。目前研究发现,Exosome内含有与细胞来源相关的蛋白质rRNA和microRNA,并且exosome能够通过生物屏障,在细胞间传递功能性核酸分子,从而发挥各种生物学功能,故exosome有望成为一种新型给药途径及基因治疗载体。Exosome携带蛋白质包括源细胞非特异性和源细胞特异性两类蛋白分子。前者可能与exosome的生物发生和生物学作用有关,主要包括:细胞溶质蛋白、参与细胞内信号转导的蛋白、各种代谢酶、热休克蛋白和四跨膜蛋白;另一类是特殊蛋白质,这类蛋白质只存在于某种特殊的细胞分泌 的exosome,而这些特定细胞源的exosome与其生物学功能有着密切联系,例如分子来源的Exosome上含有MHCII类分子。
二, Exosome 提取
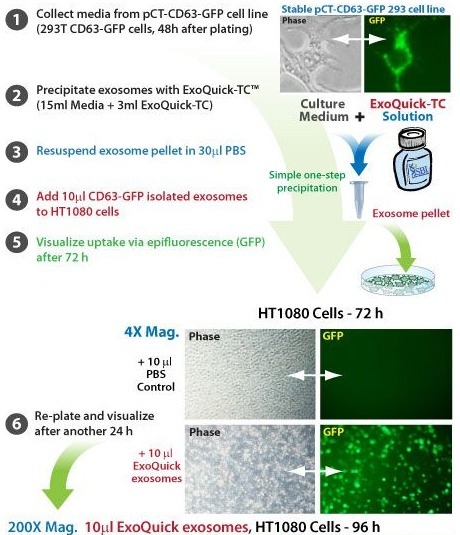
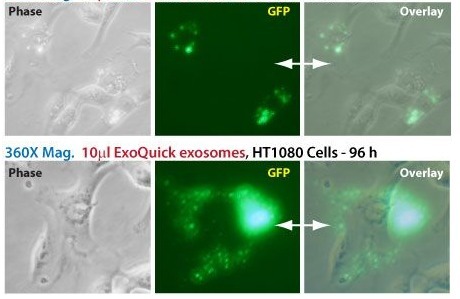
Exosome是由活细胞分泌的,它是一种亚细胞成分,组要成分是磷脂双分子和携带的膜性分子,其界定依据形态学和生物化学及提取方式不同细胞源的exosome是不同的,这些不同的理化性质有利于exosome的提取。从体外培养的细胞中分离和提取exosome的主要方法是高速离心法,这种方法能分离出大的碎片和已经死亡细胞,然后再通过超速离心法分离 提取exosome 最后利用糖梯度,使脂质囊性质的exosome漂浮于上面。具体来说,Exosome的研究方式是分离/捕获小囊泡,并拷问它所携带的货物。就目前而言,人们多采用超速离心、磁珠免疫捕获、沉淀或过滤的方法,对exosome进行前期的分离。之后利用电镜来分析其大小和形态,利用流式细胞仪来
分析细胞表面标记,通过Western blot和ELISA等方法对蛋白进行分析,或通过qPCR和新一代测序(NGS)来分析RNA。调查发现,在分离exosome时,约有56%的人采用超速离心法,说明这种方法仍是目前的金标准方法。不过这种方法缺点也不少:耗时耗力,往往需要8-30个小时;每次最多只能处理6个样品;需要大量的起始材料;产量不高。商业化的exosome提取试剂盒已经上市,更为简单省事。
1.超速离心法
将欲提取的细胞培养上清液10ml,在4 ℃的环境下,300×g 10min ,2000×g 20min,弃沉淀,去除细胞;然后l0,000×g 30min ,弃沉淀,去除亚细胞成分;再用10,000×g 60min,弃掉上清液,最后所得沉淀既为exosome,用30ml PBS 溶液重新悬浮沉淀物,混匀后再以10,000×g 60min,用 l ml PBS溶液悬浮沉淀物提纯的exosome溶液分别装入eppendorf 管内,置于-80℃冰箱内保存备用。
2.磁珠
超速离心法既耗时又费力。现在您可以通过使用灵活可控的总外泌小体分离试剂,从不同的起始样本中方便地富集完整的外泌小体。这些试剂及其配套的试验方案完美适用于广泛的实验计划,包括小输入样本量和多种样本处理实验。 从培养细胞中富集的总外泌小体(使用总外泌小体分离试剂或超速离心)可以通过免疫磁性捕获法进一步纯化为亚组分。可使用基于Dynabeads?的CD63特异性试剂,或将链霉亲和素试剂与特定的生物素化抗体结合使用,可基于表面抗原的免疫反应纯化得到任何所需的亚组分。
三, Exosome 分析
在下游分析方面,分离纯化出来的exosome可以做蛋白,也可以做RNA(microRNA和LncRNA),36%的研究人员通过Westernblot或其他方法来鉴定蛋白,29%的人员利用qPCR对microRNA表达谱进行分析,9%利用芯片进行microRNA表达谱分析。同时,新一代测序的用户也不少,13%的人员利用NGS开展microRNA/小RNA研究,9% 开展mRNA研究。此外,目前的大部分工作还是停留在科研阶段,后续的生物标志物开发和验证不多,而诊断和疗法的开发就更少。Razvi认为,exosome的定性和定量研究是个快速发展的市场。同时,循环生物标志物的市场也存在着机遇和挑战。不过,无创产前检测技术的成功让人们相信,循环生物标志物有望在肿瘤及其他疾病的诊断上发挥作用。
1.蛋白分析
(1)SDS-PAGE:通过SDS-PAGE电泳可以分析得到的Exosome中蛋白的含量及种类。
(2)Western-Blot:通过Western-Blot可以检测Exosome中特定的蛋白表达情况。
(3)2-DE等蛋白组学分析:可以了解Exosome中不同蛋白的表达、数量情况
2. 透射电镜
通过透射电镜可以分析Exosome的大小、形态等,再结合免疫标记可以很清楚的分析特定指标在Exosome表达的部位。
3.基因水平
(1)Real-Time PCR:通过PCR可以分析需要研究的指标的表达量
(2)转录组分析:通过测序或者芯片,分析Exosome不同基因的转录水平
(3)miRNA :通过测序或者芯片,检测与Exosome相关的miRNA的表达情况,研究特定的miRNA
(4)lncRNA分析:通过测序或者芯片,检测与Exosome相关的lncRNA的表达情况,研究特定的lncRNA与Exosome共同调控某种疾病的关系
四, Exosome中RNA的分离
1.切体隔离
增长切体无血清培养基的细胞。因此,任何血清细胞培养液中添加的外来应耗尽120万个晚上XG离心在4 ° C后才能使用。将细胞悬液锥形管。
在4 ° C沉淀细胞,离心10分钟300 XG。
转移上清超速离心机管,如果不彻底全面加入PBS。
样品16 500 XG离心20分钟,4 ° C至进一步去除细胞和细胞碎片。
通过0.2微米过滤除去大于200纳米的颗粒过滤上清液。
过滤上清液转移到新的超速离心机管和120 000 XG 70分钟前,超速离心机密封管在4 ° C至颗粒的外来体。
弃上清。
最大的外切体检索,悬浮切体充实ED颗粒多次在一个适当的缓冲体积小(〜3 × 50μL)。这个缓冲区取决于以下的切体隔离计划的下游实验。例如,裂解液用于蛋白质和RNA的分离,PBS是用于电子显微镜和流式细胞仪和功能的研究介质可能是首选。
注;外来体也可以从不同的体液,如血浆,使用相同的过程,作为细胞培养基中分离。对于粘性液体,它可能是必要的,用PBS稀释的样品离心和过滤步骤之前的。在上述5点的离心速度,它可以增加至29500 XG,第7点中的离心可以延长至90分钟18。
如果样品需要进一步纯化的外切体颗粒可漂浮在蔗糖梯度和外来将主要分数representing一个密度1.13-1.19克/毫升2。
2.切体识别电子显微镜
为了进一步消除污染蛋白,重悬在120 000 XG 70分钟,在4 ° C至重新沉淀外来的外切体的丰富沉淀,PBS和超速离心机。
的蛋白分离和总蛋白测定样品的小等分。确保只有一小部分样品裂解和蛋白质测量,并保存完整的外来体,解决的PBS,单独的冰或在-80℃为进一步的实验。
将在PBS重悬的完整的外来exosomal蛋白质约10微克,一个下降,一个封口膜。然后,用血管钳,轻轻的位置上每一滴30-60分钟的顶部formvar碳包覆镍网格。保证网格定位涂层的一面面临下降含外来。
将三滴,每30μL的PBS,在T他封口膜和洗网格,按顺序定位的PBS液滴上的电网和使用吸油纸之间。使用吸油纸轻轻只是抱着它不涂面积接触,密切合作,以电网侧。
修复存款样品的封口膜下降了2%多聚甲醛,并放置在顶部的10分钟下降的网格。
重复洗涤步骤中的第4点,前一个合适的抗体免疫。常用的抗体是抗CD63和抗MHCⅡ类。电子显微镜也可以不免疫作为外来体的大小和形态上,完全可以识别基于。但是,我们建议,评估的大小,形态和为一个更确凿的验证的膜蛋白的存在。
网格传输选择的主要抗体30μL下降,孵育40分钟。洗净重复第4点,但在PB中使用0.1%的牛血清白蛋白S代替的PBS单独。
重复第7点,但与10纳米金标记的第二抗体和单用PBS洗。
修复后下降了2.5%戊二醛中加入的封口膜样品,孵育10分钟下降顶部的网格。重复第4点的洗,但使用去离子水液滴,而不是三个水滴的PBS。
对比样品加入下降2%醋酸铀的封口膜,下降为15分钟的顶部,并培育网格。
嵌入下降了0.13%甲基纤维素和0.4%的醋酸铀的封口膜样品,孵育10分钟下降顶部的网格。
删除多余的液体,然后轻轻地使用吸油纸的定位与涂边格在一张纸上,让空气干燥5分钟。
用电子显微镜检查的筹备工作,或存储在网格中的电网,为今后的工作。
3 由流式细胞仪的外切体的表征
作为外来太小,由目前的流式细胞仪设备检测,有必要先绑定外来抗体包被的磁珠( 图1)。这些珠子可以购买一个现成的产品,或选择的抗体在实验室。根据exosomal细胞来源,不同的抗体可以配上珠可以磁或乳胶字符。我们目前使用的抗MHCII类或抗CD63的包被的磁珠,这种分析。对于使用“国产”的抗体包被的磁珠,我们使用4微米乳胶具有抗CD63抗体包被的磁珠。25μL4微米乳胶珠(30 × 10 6珠)100μL的MES缓冲的两倍,3 000 XG15-20分钟,洗净,在100μL的MES缓冲溶解沉淀。准备抗体的混合物,其中包含一个体积等于12.5微克抗体与相同体积的MES缓冲。添加珠抗体的混合物,在室温下孵育过夜搅拌。抗体包被的磁珠洗净,用PBS(3000 20分钟XG)三次沉淀溶于100μL存储缓冲区(与终浓度为300 000珠/μL)。
对于每个样本(每个抗体),继续与卷等于30微克exosomal蛋白质的最低%〜100 000抗体包被珠(PBS中解决了完整的外来)。
孵育外来珠,在一个总体积300μLPBS过夜,在4 ° C下轻柔的动作。
加入300μL200毫米甘氨酸和孵化30分钟座。
两次洗涤缓冲液的切体珠复合物(1-3%血清的PBS),10分钟600 XG洗净。
孵育50μLIgG抗体的外切体珠复合物4 ° C。在洗涤缓冲液洗净切体珠复合物,在第5步中所述的两倍。
添加90μL洗涤缓冲液和10μL抗体的选择(理想的抗CD9,抗CD63或CD81的反)的切体珠复合物和40分钟,轻柔的动作下孵育。在洗涤缓冲液的切体珠复合物在第5步中所述的两次洗净。
加入300μl洗涤缓冲液,并用流式细胞仪采集数据。
如上所述,不同的珠子可以使用,如协议或磁珠所述的乳胶珠。如果用来代替磁珠,请注意,该协议是略有不同。阻塞步骤(4点)是不是必需的,是由放置在一个磁性的立场,而不是一个离心管进行洗。
“自制”的抗体包被的磁珠使用的存储缓冲区,包含0.1%甘氨酸和azid在PBS,pH值7.2,0.1%钠。
更重要的是,确保使用流式细胞仪洗涤缓冲液(1-3%血清的PBS)外切体耗尽血清,以避免任何血清外来污染分析。
请注意,使用抗体加上珠的切体的表征时,重要的是要承认,这仅仅是一个特定的亚群,特定于所使用的抗体,即分离并鉴定。
4.切体检测用Western blot
Western印迹是一个行之有效的方法,我们不会细讲就方法本身,但重点放在一个合适的蛋白分离前的印迹和使用不同的抗体的重要性。
溶解蛋白裂解液的选择外切体颗粒,并彻底吹打,旋涡混合。要进一步裂解的外来体,超声水浴中3 ×5分钟之间的旋涡混合样品。最后,在室温下5分钟离心样品13 000 XG,将上清转移到一个新的Eppendorf管。
Measu重新选择的方法总蛋白和负载20-50微克的蛋白质,每口井。
凝胶电泳和电泳分离和转移的蛋白质。
座和洗膜,然后再执行对在外来丰富的蛋白质免疫。
检测化学发光数字成像系统和分析软件的特定蛋白质。
至于有没有切体的特异性标志物,在外来丰富的蛋白质,从各个不同的细胞起源,是常用的外切体检测。这些tetraspanins(如CD9,CD63和CD81),细胞骨架相关蛋白(如ezrin)和多泡的生物合成(如TSG101和ALIX)涉及的蛋白质,如蛋白质。其他蛋白质也常用于外来检测Flotillin,HSC70和不同的Rab蛋白等,但也有特定的蛋白质,如A33(肠上皮细胞)的外来细胞中CD3(T细胞)和MHCⅡ类(抗原呈递细胞)。因此,根据外来体是由什么类型的细胞进行检测标记发布可能会有所不同。
由于其他车厢的细胞也能产生水泡,这是进一步建议,以确定这些车厢,如内质网(如calnexin和GRP78)和高尔基体(如GM130)的蛋白质的存在。因此,这些蛋白质的缺乏表示没有或很少污染样品中的其他车厢的囊泡研究。
5. exosomal RNA和RNA分析的分离
切体颗粒溶解在RNA裂解液的选择和执行RNA的提取。根据下游实验不同的RNA分离试剂盒可用于,但基于列的方法提供了更广泛的RNA样品。目前,我们正在使用由ExiqonmiRCURY RNA分离试剂盒,但可能适合在SC上其他套件ientific问题就在眼前。
在进行RNA的分离是很重要的工作在无RNase的环境。因此,使用核酸和核酸免费枪头和擦拭工作台和设备,无污染物和核糖核酸酶。
RNA的提取,使用miRCURY RNA提取试剂盒,溶于350μL裂解液的切体颗粒,并执行旋涡混合15秒。
加入200μl95%乙醇和10秒的旋涡混合的。
放置在一个收集管一列,并转移裂解外来列和离心1分钟14 000 X G.
包含exosomal RNA和离心1分钟14 000 X G.列加入400μL洗涤液洗三次
离心2分钟14 000 XG,以确保该列是干的,并放置在一个无RNase Eppendorf管干栏列。
加入50μL洗脱液列和2型离心机 200 XG分钟,其次是1分钟14 000 X G.
继续分离出的RNA,或存放在-80 ° C。
五, Exosome 相关质粒
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








求原文,这翻译的没看懂。。
48
简单明了,新颖启发
95
这篇资讯带给我们新知识,启发新思维,不论是科研还是临床工作都有很大的帮助。。。
85
文章中很多地方都表达的不准确,语句不通,感觉是机器自动翻译的结果,求准确翻译或英文原文
1
#Exosome#
28
太有用了!
164
学习了,我们实验室正好在做这方面的实验
119
#检测方法#
22
最热的领域
61
不错,很有用~
83