Eur J Intern Med:大麻改善晚期癌症患者生存质量:真相究竟是什么?
2018-03-24 Jenny 肿瘤资讯
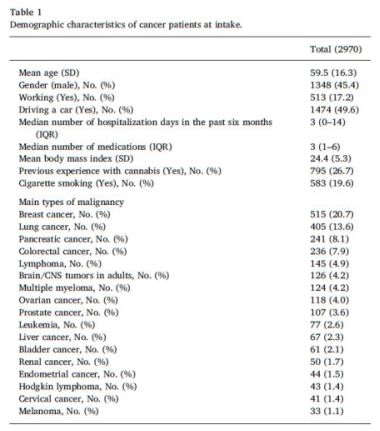
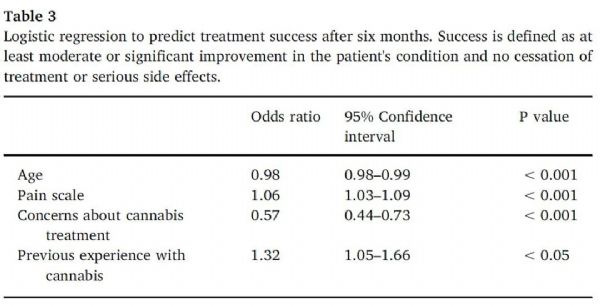
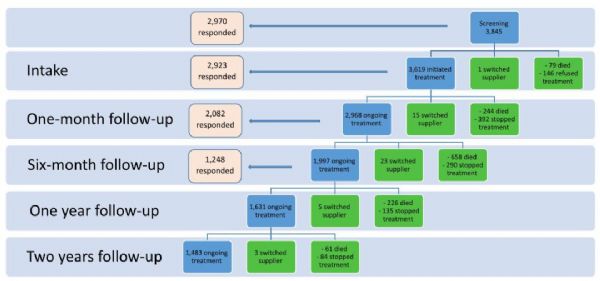
2018年3月《European Journal of Internal Medicine》欧洲内科医学杂志最新发表的文章“大型前瞻性研究——医用大麻在癌症人群中的安全性和疗效” ,首次证实了几十年来关于大麻在癌症患者中的获益,大麻对癌症患者可能是安全有效的姑息治疗。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#生存质量#
41
#患者生存#
38
#晚期癌症患者#
34
谢谢分享.学习了!
96
需要更多的实验数据支持!任何事物都有两面性.
102
#大麻#
35
#癌症患者#
36
#Med#
31
阅
93
阅
80