J Neurol Neurosur Ps:复发性和进行性多发性硬化症风险的影响因素
2021-05-24 MedSci原创 MedSci原创
相同的环境和生活方式因素会影响复发和进行性发作的MS,这些结果支持以下观点即不同临床表型的MS具有共同的潜在致病机制。
对于多发性硬化症(MS)不同的临床病程是否是致病机制不同的结果,因为不同致病机制具有不同的危险因素;以及所有MS临床表型是否是相似的潜在致病机制的不同表现,这些问题一直存在争议。

近日,神经病学领域权威取杂志Journal Of Neurology Neurosurgery And Psychiatry上发表了一篇研究文章,研究人员旨在探究环境危险因素及其与人白细胞抗原DRB1 * 15:01的相互作用在复发发作和进行性发作的MS发病中的作用。

研究人员了瑞典2项基于人群的病例对照研究,纳入了7520例复发发作MS病例,540例进行性发作的MS病例和11386名按年龄、性别和居住地区进行匹配的对照者。研究人员采用Logistic回归用于估计具有95%CI的OR,以反映不同MS表型与许多环境和生活方式因素之间的关联。DRB1 * 15:01等位基因与环境危险因素之间的相互作用在添加性标尺上进行了评估。
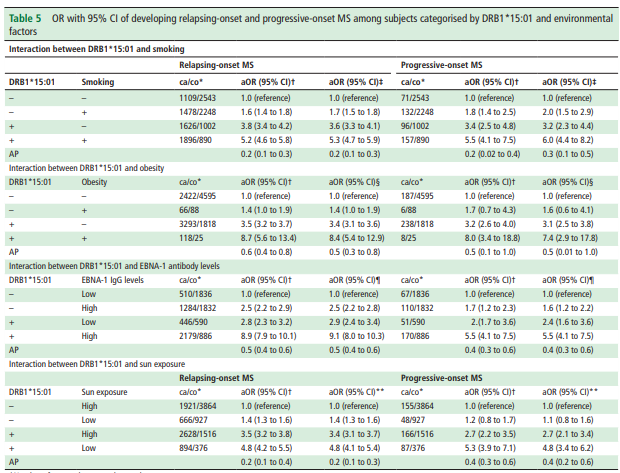
研究人员发现与发生MS风险相关的所有环境和生活方式因素均适用于复发性MS和进行性MS。吸烟、肥胖和EB病毒核抗原1(EBNA-1)抗体水平与两种表型的MS风险增加相关,而吸烟、饮酒和日光照射与其风险降低相关。无论临床表型如何,DRB1*15:01与吸烟、肥胖、EBNA-1抗体水平和日光照射之间的添加性相互作用均会增加MS风险。
由此可见,相同的环境和生活方式因素会影响复发和进行性发作的MS,这些结果支持以下观点即不同临床表型的MS具有共同的潜在致病机制。
原始出处:
Anna Karin Hedström.et al.Factors affecting the risk of relapsing-onset and progressive-onset multiple sclerosis.Journal Of Neurology Neurosurgery And Psychiatry.2021.https://jnnp.bmj.com/content/early/2021/05/13/jnnp-2020-325688-0
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#硬化症#
35
#复发性#
24
#Neurol#
22
#进行性#
34
#多发性#
30
#ROS#
26
#影响因素#
0