病例分享:突发胸痛,D二聚体升高,病因竟是……
2018-02-20 大漠落日 医学界心血管频道
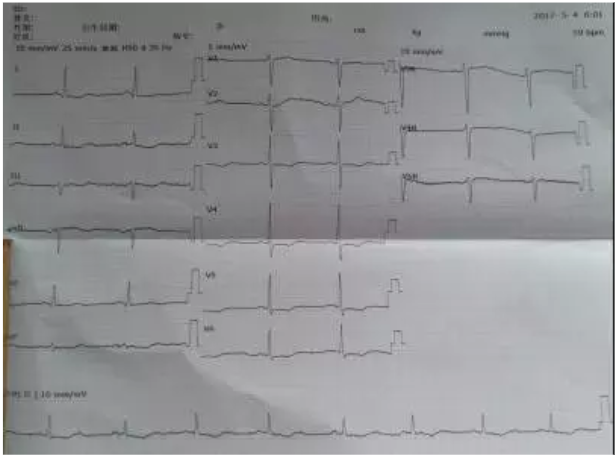
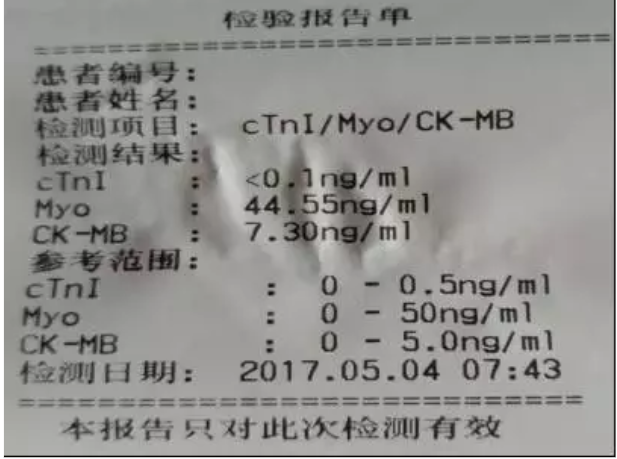
患者,男,45岁,既往患有高血压病,因突发剧烈胸痛4小时前来就诊,发病后一小时在当地医院查心电图。

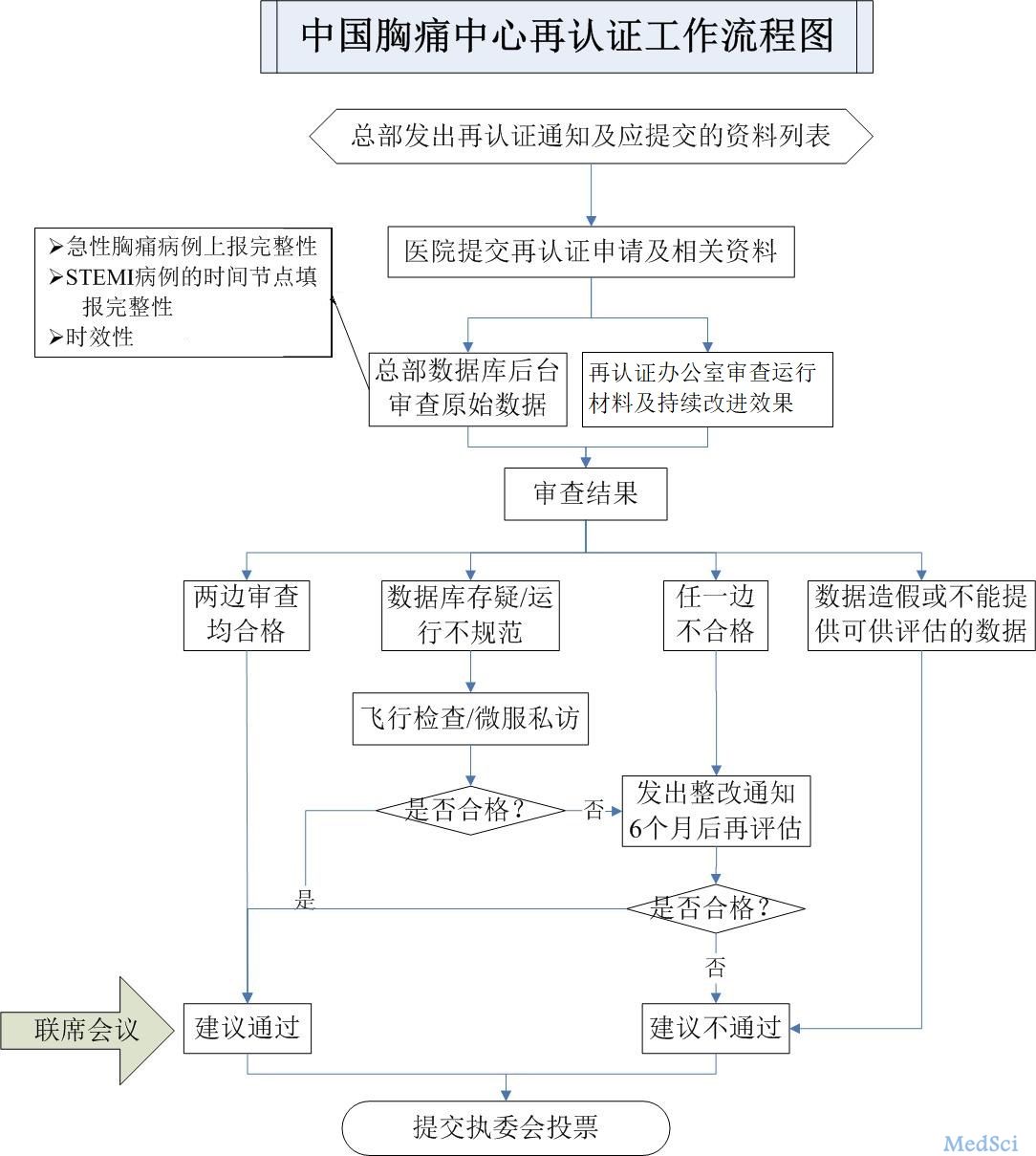
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#二聚体#
41
#突发胸痛#
44
学习了感谢分享
76
学习了.谢谢分享
75
好棒的分析
75
好病例分析.学习了.
61
阅
63