Blood:高选择性BTK抑制剂zanubrutinib用于CLL/SLL的活性和安全性
2019-07-25 MedSci MedSci原创
Zanubrutinib是Bruton酪氨酸激酶(BTK)的一种高效、高选择性抑制剂。本研究是首次在人类中开展的开放性、多中心的I期研究,第1部分(3+3)剂量递增队列招募复发/难治性B细胞恶性肿瘤患者,予以zanubrutinib 40mg、80mg、160mg或320mg,1/日,或160mg 2/日。第2部分(扩展)为特定疾病的队列,包括初治或难治性/复发性慢性淋巴细胞白血病/小淋巴细胞淋巴
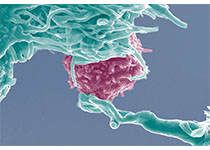
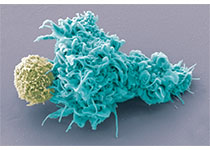
Zanubrutinib是一种有效的选择性BTK抑制剂,比依鲁替尼的选择性更强、脱靶效应更低
对于复发性/难治性或未治疗过的CLL患者,zanubrutinib治疗耐受性良好、疗效佳
摘要:
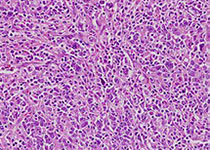
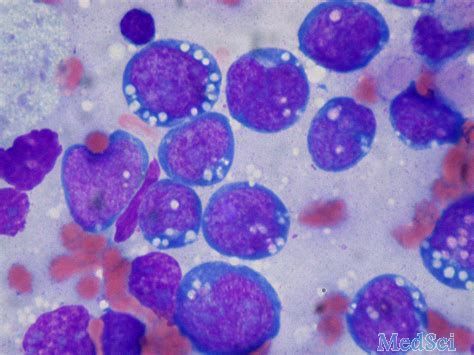
Zanubrutinib是Bruton酪氨酸激酶(BTK)的一种高效、高选择性抑制剂。本研究是首次在人类中开展的开放性、多中心的I期研究,第1部分(3+3)剂量递增队列招募复发/难治性B细胞恶性肿瘤患者,予以zanubrutinib 40mg、80mg、160mg或320mg,1/日,或160mg 2/日。第2部分(扩展)为特定疾病的队列,包括初治或难治性/复发性慢性淋巴细胞白血病/小淋巴细胞淋巴瘤(CLL/SLL)。
主要结点是安全性、耐受性和明确最大耐受剂量(第1部分)。次要结点包括药代动力学/药效学和初步疗效.
剂量递增队列和CLL/SLL队列共招募了144位患者。未观察到剂量限制性毒性。各剂量时,BTK在外周血单个核细胞中的平均占用率>95%。160mg 2/日时淋巴结活检样本中BTK持续完全占领的发生率高于320mg 1/日(89% vs 50%,p=0.0342)。
因此,选择160mg 2/日进行进一步的研究。中位随访13.7个月(范围0.4-30.5),89例(94.7%)CLL/SLL患者仍在研究中。毒副反应以1/2级为主;中性粒细胞减少是唯一观察到的3/4级毒性(2位)。一名患者发生3级皮下出血。
在78位疗效可评价的CLL/SLL患者中,总缓解率为96.2% (95% CI, 89.2-99.2)。估计12个月无进展存活率为100%。
综上所述,zanubrutinib用于CLL/SLL患者可获得较好的活性,而且副作用发生率低。
Constantine Si Lun Tam, et al.Phase 1 study of selective BTK inhibitor zanubrutinib in B-cell malignancies and safety and efficacy evaluation in CLL. Blood 2019 :blood.2019001160; doi: https://doi.org/10.1182/blood.2019001160
本文系梅斯医学(MedSci)原创编译,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#选择性#
27
#抑制剂#
33
#高选择性#
27
#BTK抑制剂#
34
#zanubrutinib#
37
#BTK#
21
#CLL/SLL#
37