Cardiovasc Diabetol:白脂素诱导糖尿病下肢外周动脉疾病血管内皮细胞向间质细胞转化
2022-05-23 从医路漫漫 MedSci原创
除了年龄、性别和遗传背景外,PAD还与其他动脉粥样硬化疾病有相似的风险因素,如吸烟和代谢综合征的组成部分,包括肥胖、糖尿病、血脂异常和高血压。
背景:下肢外周动脉疾病(PAD)是供应腿部的外周动脉的动脉粥样硬化性闭塞性疾病。根据最近的系统回顾,全世界有2.38亿人患有PAD,这被认为是一个全球性的健康问题,导致残疾调整寿命年数、生命折损年数和残疾生活年数增加。PAD患者不仅要忍受间歇性跛行或非典型缺血性腿痛导致的生活质量下降,而且还有较高的死亡率,因为PAD也是未来心血管事件的有力预测因素,如心肌梗塞和中风。除了年龄、性别和遗传背景外,PAD还与其他动脉粥样硬化疾病有相似的风险因素,如吸烟和代谢综合征的组成部分,包括肥胖、糖尿病、血脂异常和高血压。因此,目前在PAD的治疗中,除了生活方式和针对上述危险因素的药物外,主要是应用血管内介入或手术,不用说,PAD的具体诊断和治疗方法是迫切需要的。过多的脂肪组织堆积是代谢综合征的一个标志,它促进了包括PAD在内的动脉粥样硬化疾病的发展。作为一个新发现的内分泌器官,脂肪组织分泌一系列的脂肪因子,如瘦素、脂肪素、成纤维细胞生长因子21(FGF21)等,参与心血管系统的代谢和功能的调节。功能失调的脂肪组织中脂肪因子的合成和分泌发生改变,导致一系列代谢性动脉粥样硬化性疾病。白脂素是profibrillin的C端裂解产物,是最近发现的一种脂肪因子,在代谢中显示出强大的调节作用。除了刺激肝脏葡萄糖生成,增加血液中的胰岛素和葡萄糖水平外,天冬氨酸还直接促进胰岛β细胞的凋亡。相应地,在糖尿病患者中检测到血浆中的天冬氨酸水平升高,表明天冬氨酸在糖尿病血管损伤中可能有促进作用。然而,在糖尿病状态下,天冬氨酸与下肢PAD之间的关系还没有被研究过。
内皮功能障碍的特点是血流介导的扩张(FMD)降低,长期以来被认为是PAD患者心血管风险的独立预测因素,并增加了踝臂指数(ABI)的预测价值,ABI是广泛用于诊断PAD的传统参数。从机制上讲,高血糖导致的晚期糖化终产物(AGEs)水平的增加诱发了活性氧(ROS)的产生,使内皮细胞产生的一氧化氮(NO)和未耦合的内皮细胞NO合酶(eNOS)活性失活,从而导致炎症,造成血管损伤。值得注意的是,与含有更多脂质的冠状动脉粥样硬化困扰相比,PAD患者的大多数下肢动脉显示内侧钙化,导致外周动脉硬化。血管钙化是一个活跃的过程,由于血管细胞的转分化,其中内皮细胞向间质转化(EndMT)主要影响内皮细胞(ECs)。在EndMT的过程中,内皮细胞之间紧密的细胞-细胞连接被破坏,其鹅卵石般的良好结构外观转换为纺锤形的纤维细胞,其中TGF-β信号通路起着核心作用。尽管EndMT被认为是内皮功能障碍的一个关键机制,但EndMT是否参与下肢PAD,以及天门冬素是否在EndMT中发挥作用仍是未知数。
目的:在这项研究中,我们招募了PAD患者,并证实血浆中阿斯匹林水平的升高与PAD的各种参数独立相关。此外,通过代谢全能筛查和细胞实验,我们证实EndMT是一个与PAD相关的重要过程,并揭示了此前未被认识到的阿斯匹林对EndMT的促进作用的分子机制,从而更新了对PAD血管损伤的认识,为今后临床上治疗和干预PAD提供了新的目标。
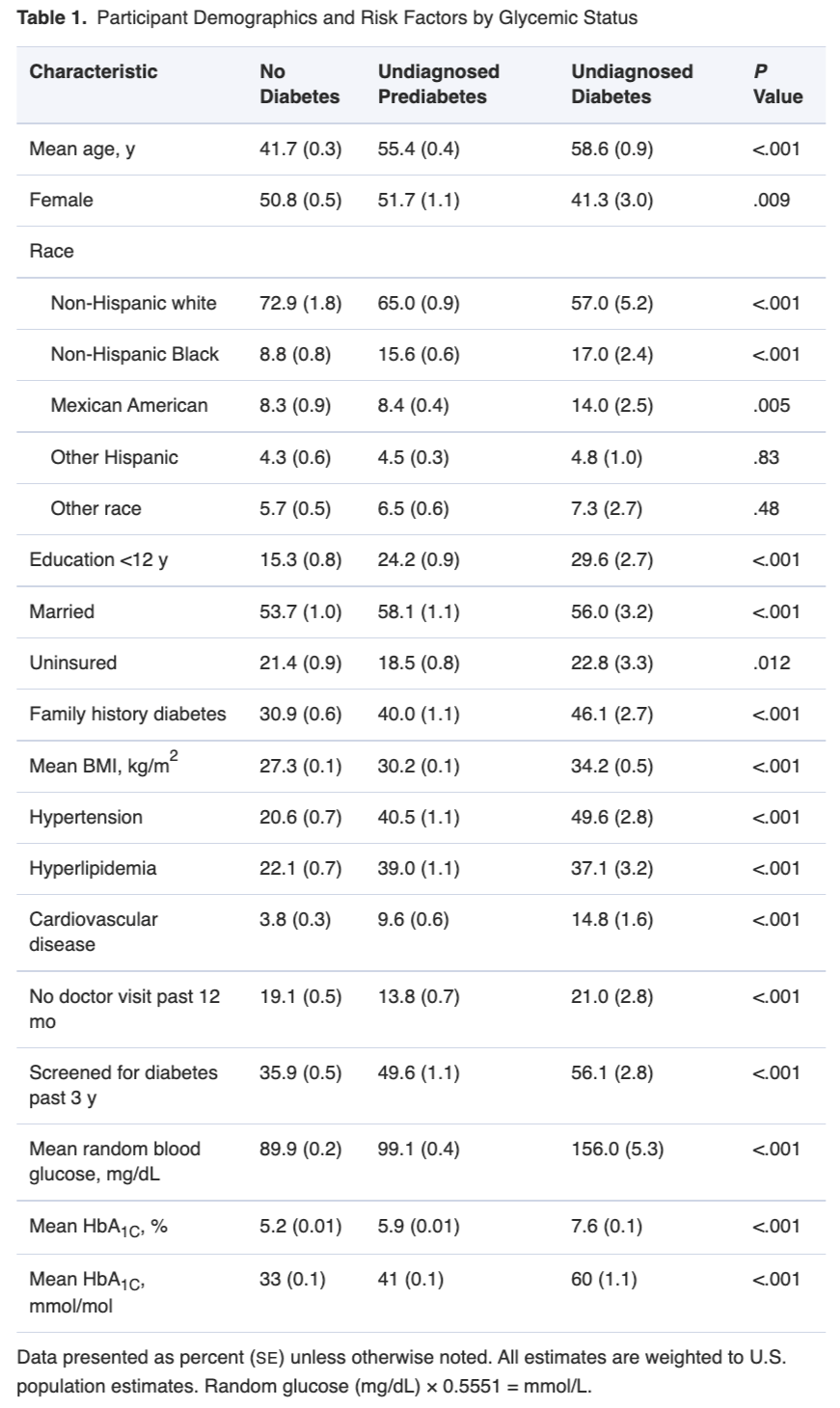
方法:招募了33名2型糖尿病(T2DM)患者(DM)、51名T2DM患者合并PAD(DM + PAD)和30名健康的正常对照(NC)志愿者,收集血样用于检测循环中的天冬氨酸水平和代谢组学筛选。使用2型糖尿病db/db小鼠的主动脉组织进行RNA测序,并用天冬氨酸处理人脐静脉内皮细胞(HUVECs),以确定其对内皮细胞向间质转化(EndMT)的影响。
结果:DM+PAD组的天冬酰胺的循环水平明显高于NC组和DM组。即使调整了年龄、性别、体重指数(BMI)和其他传统的PAD危险因素,循环中的天冬氨酸水平与踝臂指数(ABI)明显呈负相关。Logistic回归分析显示,天冬氨酸是PAD的一个独立风险因素,接收器操作特征(ROC)曲线确定天冬氨酸对区分PAD具有良好的敏感性(74.5%)和特异性(74.6%)。代谢组学的数据显示,PAD患者的肌成纤维细胞在胶原蛋白生产中具有典型的从头合成氨基酸的特征,并且在db/db小鼠的主动脉组织中出现了TGF-β信号通路的激活。阿斯匹林以TGF-β依赖性的方式直接诱导HUVECs的EndMT,因为TGF-β信号通路抑制剂SB431542消除了阿斯匹林对EndMT的促进作用。
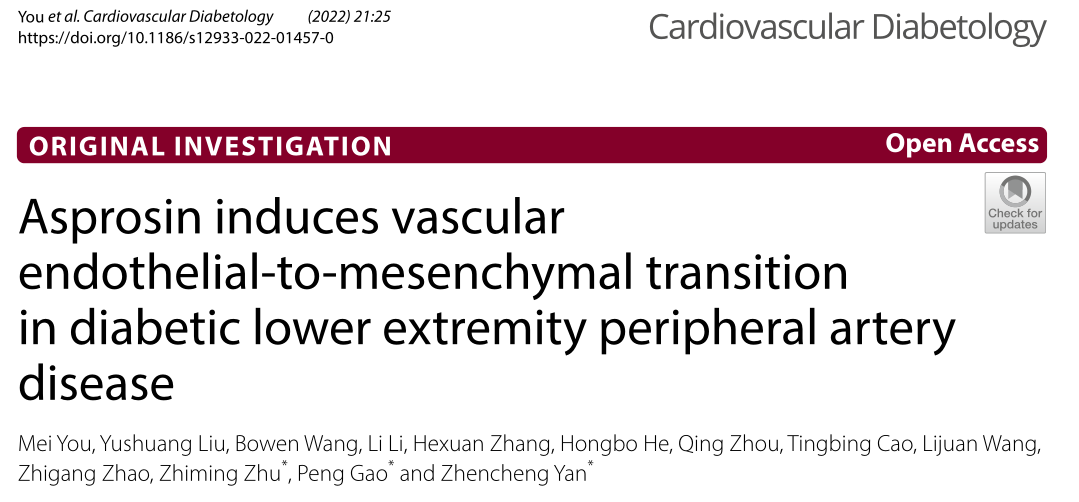
表1 不同组别中受试者的人口统计学和临床数据
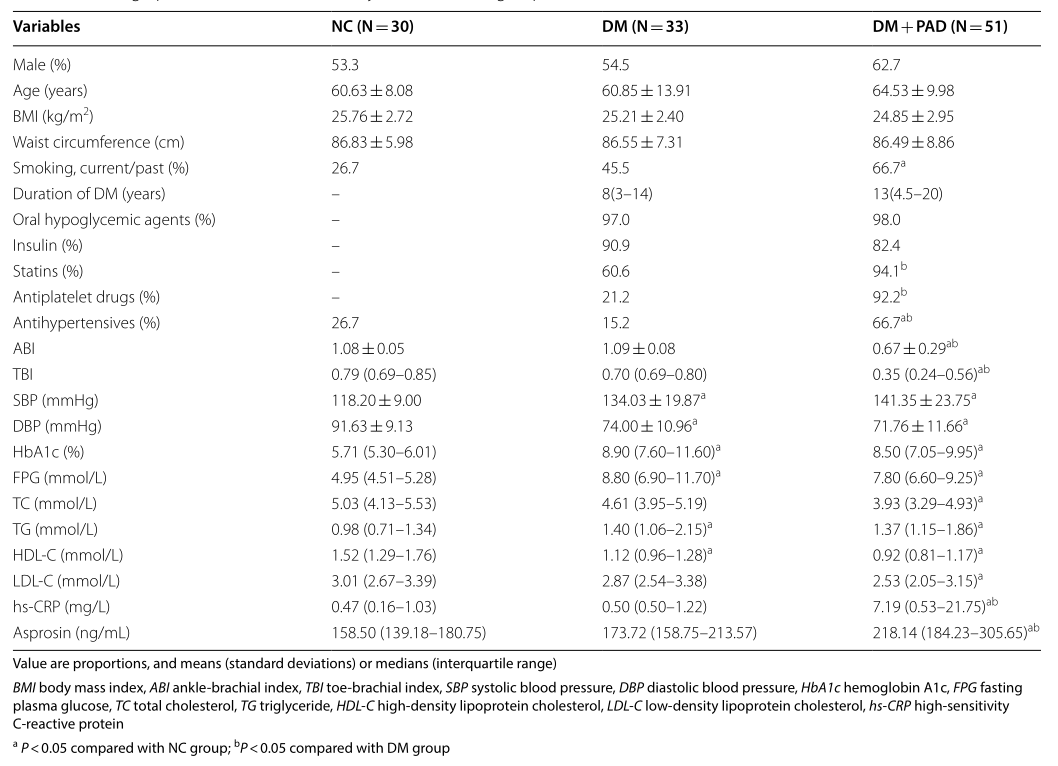
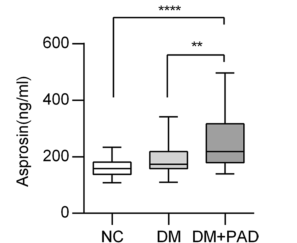
图1 NC、DM和DM+PAD组的循环天门冬素水平。***P < 0.001, **P < 0.01, 数据为中位数,最大和最小值。
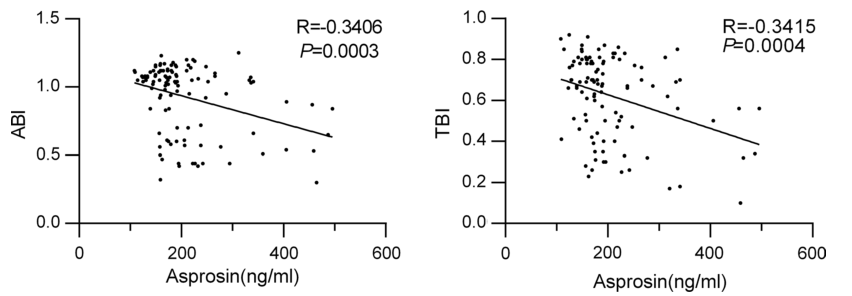
图2 所有受试者的循环阿斯匹林水平与ABI/TBI之间的相关性
表2 所有受试者的循环阿斯匹林水平与ABI和TBI的相关性
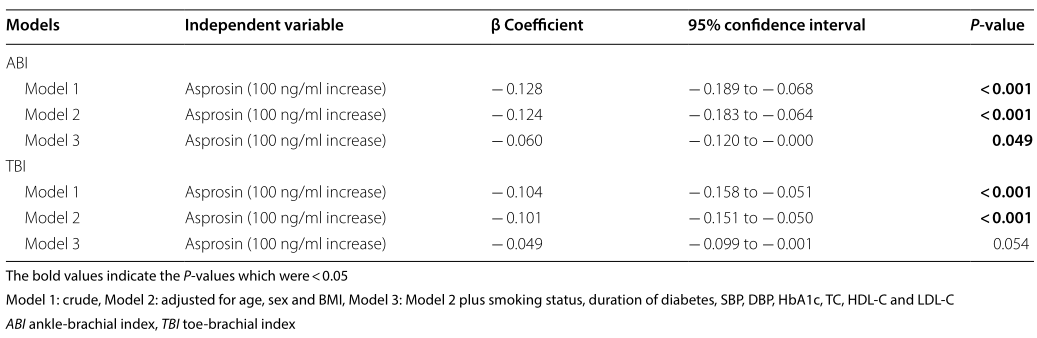
表3 通过逻辑回归分析,循环中的阿斯匹林水平与PAD的关系

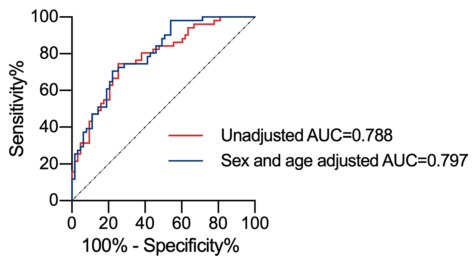
图3 所有受试者的阿斯匹林的接收操作特征(ROC)曲线。曲线显示了天冬氨酸测定对PAD的判断能力。AUC 曲线下的面积
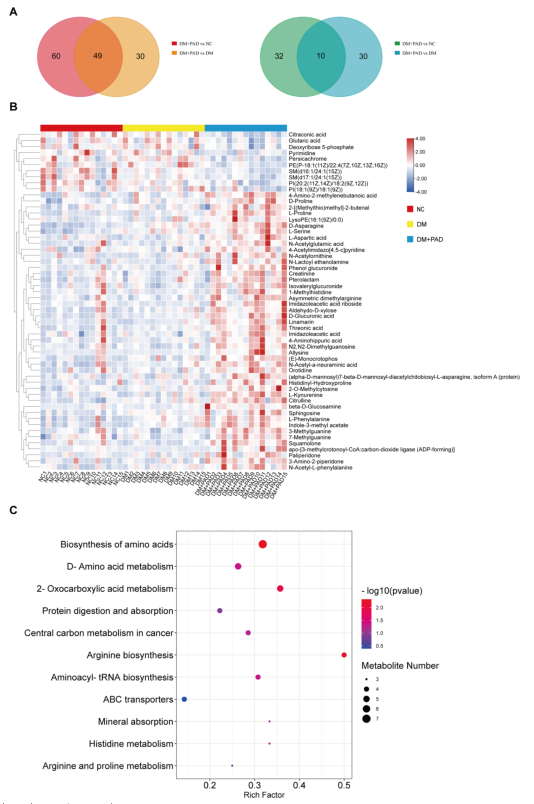
图4 对参与者血清的代谢组学分析。A 维恩图显示了与DM或NC组相比,DM+PAD组中上调(左)和下调(右)代谢物的数量。B 与DM组和NC组相比,DM+PAD组同时存在59种不同表达的代谢物的热图。C 59种差异表达的代谢物的KEGG途径分析
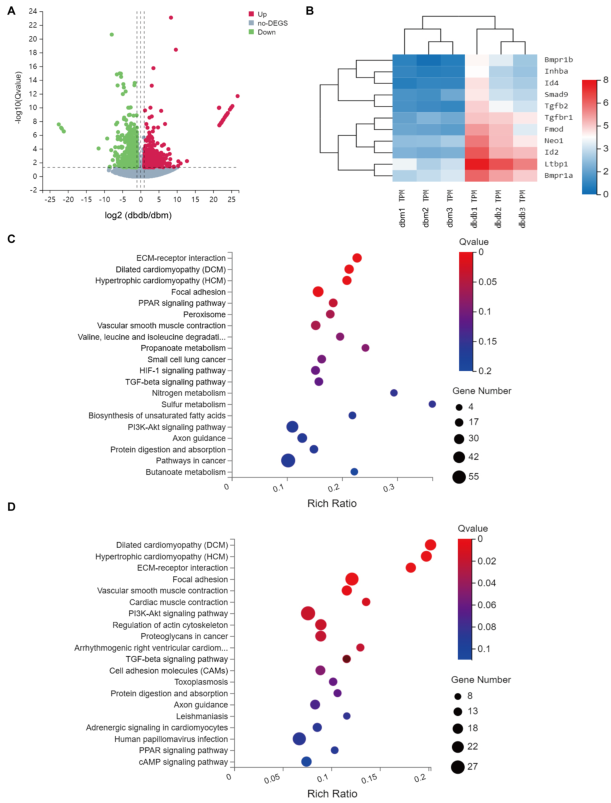
图5 RNA测序数据的分析结果 (A) 从db/db或db/m小鼠分离的主动脉差异表达基因的火山图(每组n = 3)。显示了1049个上调(红色)和1043个下调(绿色)的基因。B 富含TGF-β信号通路的差异表达基因的热图。基因符号显示在右边(每组n = 3)。C 对2092个差异表达的基因进行KEGG途径分析。D 对1049个上调表达的基因进行KEGG途径分析
结论:循环中的天冬氨酸水平升高是下肢PAD的一个独立危险因素,并可能作为一种诊断标志。从机制上讲,天冬氨酸直接诱导EndMT,通过激活TGF-β信号通路参与血管损伤。
原文出处:You M, Liu Y, Wang B, et al.Asprosin induces vascular endothelial-to-mesenchymal transition in diabetic lower extremity peripheral artery disease.Cardiovasc Diabetol 2022 02 15;21(1)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#BET#
37
#ASC#
54
#DIA#
44
#下肢外周动脉疾病#
54
#血管内皮细胞#
65
#外周动脉#
50
#学习#
55