Int J Clin Oncol:前期接受醋酸阿比特龙和多西他赛治疗的转移性去势敏感前列腺癌患者的真实结果和风险分层
2022-06-27 AlexYang MedSci原创
评估了接受两种前期治疗方法的转移去势敏感性前列腺癌(mCSPC)患者的临床结果情况。
前列腺癌(PCa)是全球第二大最常见的恶性肿瘤,也是全球男性癌症死亡的第六大原因。前列腺特异性抗原(PSA)筛查的广泛实施引起局部PCa发病率增加和转移性PCa的减少。在2012年,美国建议反对基于血清PSA的常规筛查后,新发转移性PCa的发病率有所增加。同时,亚洲的PCa患者在诊断时的临床阶段通常比西方患者更高。

近期,来自日本的研究人员在《Int J Clin Oncol》上发表文章,评估了接受两种前期治疗方法的转移去势敏感性前列腺癌(mCSPC)患者的临床结果情况。
研究人员调查了2014年至2021年期间接受雄激素剥夺疗法加前期醋酸阿比特龙(ABI)或多西他赛(DOC)治疗的301名mCSPC患者的医疗记录。之后,进行倾向性评分匹配(PSM)来比较生存结果,并对二次进展的风险因素进行了亚组分析。
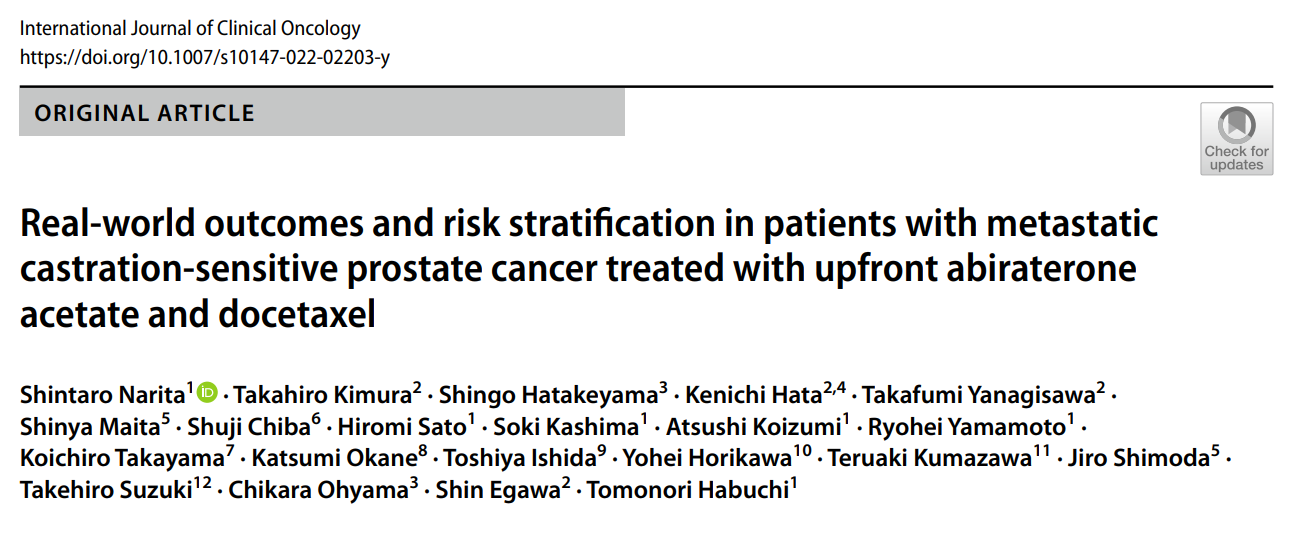
研究中,共有95名患者接受了前期DOC治疗,而206名患者接受了前期的ABI治疗。PSM后,ABI组的无进展生存期明显优于DOC组[危险比(HR),0.53;95%置信区间(CI),0.34-0.82]。ABI组的二次无进展生存期(PFS2)有比DOC组长的趋势,但没有统计学显著意义(HR,0.64;95%CI,0.33-1.22)。两组之间的总生存期(OS)没有明显差异(HR,0.92;95% CI,0.42-2.03)。在亚组分析中,与前期DOC相比,前期ABI治疗在年龄≥75岁的患者中具有明显较好的PFS2(P=0.038)。二次进展的四个风险因素(原发Gleason 5、肝转移、高血清碱性磷酸酶水平和高血清乳酸脱氢酶水平)可成功地将患者分层为三个风险组。
前期DOC或ABI治疗后mCSPC患者的生存结果情况
综上所述,前期ABI治疗比前期DOC治疗具有更好的无CRPC生存期;然而,两组之间的PFS2或OS没有明显差异。因此,基于预后风险因素的个性化治疗,有可能有利于那些接受前期强化治疗的mCSPC患者。
原始出处:
Shintaro Narita , Takahiro Kimura , Shingo Hatakeyama et al. Real-world outcomes and risk stratification in patients with metastatic castration-sensitive prostate cancer treated with upfront abiraterone acetate and docetaxel. Int J Clin Oncol. Jun 2022
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Oncol#
47
#风险分层#
50
#醋酸阿比特龙#
44
#转移性#
50