ACC:室上性心动过速对急性肺栓塞患者结局的影响
2022-04-06 Shirley MedSci原创
急性肺栓塞 (PE)的临床表现包括呼吸困难、包括SVT在内的心动过速、氧饱和度下降、胸痛、晕厥、低血压等。关于 SVT 对 PE 住院临床结果的影响程度的文献有限。
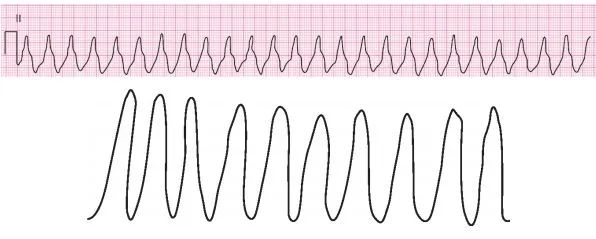
背景:室上性心动过速(SVT) 是临床上常见的一种快速性心律失常, 涉及的部位包括房室结、传导附加束、心房和窦房结等,是一种住院人群中常见的快速性心律失常。
急性肺栓塞 (PE)的临床表现包括呼吸困难、包括SVT在内的心动过速、氧饱和度下降、胸痛、晕厥、低血压等。关于 SVT 对 PE 住院临床结果的影响程度的文献有限。

方法:使用从 2016 年至 2018 年联合国家住院患者样本 (NIS) 数据库获得的数据设计了一项回顾性队列研究。使用国际疾病分类代码第十修订版 (ICD-10) 确定患有肺栓塞的成年患者(年龄 >18 岁),并根据 SVT 的存在分为两组。主要结果是死亡率、住院时间 (LOS) 和总住院费用。次要结局包括心源性休克、低血压、心动过缓和急性肾损伤。使用多元线性和逻辑回归来调整混杂因素。
结果:共有 372,729 名成人因急性 PE 住院,其中 1.6% 与 SVT 相关。SVT 的存在使死亡率增加 1.5 倍(6.9% 对 2.9%,AOR -1.54,95% CI:1.19-2.01,p-0.001),并使 LOS 增加 1.6 天(6.63 天对 4.33 天) ,调整后的平均差;1.58 天,95%CI;1.23 - 1.94,p <0.001)。两组之间的总电荷没有显着差异。SVT 的存在与心源性休克的几率增加相关(3.42% vs 1.13%,AOR-1.83,95% CI;1.28 - 2.63,p-0.001)、低血压(4.22% vs 7.77%,AOR-1.41,95% CI ; 1.13 - 1.77, p-0.003) 和急性肾损伤 (19.56 vs 12.01, AOR - 1.24, 95%CI; 1.05 - 1.46, p- 0.013)。两组之间的心脏骤停、心动过缓或中风没有差异.
结论:因 PE 住院的患者出现 SVT 与死亡率和住院时间增加以及心源性休克、低血压和急性肾损伤的不良临床结果相关。需要对此主题进行进一步的前瞻性研究,以更好地指导管理患者。
讨论:PE后出现SVT并不少见,但是常常因为持续时间短而被忽略。SVT本身就有可能增加低血压或者心动过缓的发生率进导致心源性休克,并且增加包括肾功能损害在内的终末器官并发症的风险,增加死亡率。因此对于这一部分患者可能需要进一步的检查和治疗,从而减少患者的住院时间和治疗费用。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#室上性心动过速#
73
很不错的研究发现,学习了,非常感谢
68
#急性肺栓塞#
66
#ACC#
38
#心动过速#
53
#患者结局#
39
学习了
0