The Oncologist:免疫治疗治疗转移性非小细胞肺癌的疗效:中东欧国家的真实世界数据
2021-08-08 yd2015 MedSci原创
这是第一个来自中东欧国家关于免疫治疗在转移性NSCLC患者中疗效的真实世界数据。
驱动基因阴性转移性非小细胞肺癌(NSCLC)目前一线或二线治疗的标准方案为免疫治疗或联合化疗。近期,来自中东欧国家的研究团队开展了真实世界研究,评估免疫治疗再转移性非小细胞肺癌(NSCLC)的疗效。相关结果发表在The Oncologist杂志上。
在2015年8月至2018年11月的研究期间,纳入66例连续接受ICIs治疗患者。其中26例患者在一线接受了ICIs(pembrolizumab)治疗,40例患者在二线接受了ICIs(atezolizumab, nivolumab, or pembrolizumab)治疗。中位年龄为64岁,55%为男性,6%患者ECOG≥2,18%患者基线有可控的脑转移。
26例一线治疗为pembrolizumab单药治疗,患者PD-L1≥50%。在二线治疗中,10%(4/40)的患者接受atezolizumab,58%(23/40)的患者接受nivolumab,33%(13/40)的患者接受pembrolizumab。二线治疗的患者中,只有25%(10/40)的患者有PD-L1表达≥50%,而大多数患者有48%(19/40)的PD-L1表达<1%,10%(4/40)的患者PD-L1表达不明。
在一线治疗中,中位随访时间为19.9个月,ORR为46%(12/26)(4例获得完全缓解[CR],8例获得部分缓解[PR]),另有27%(7/26)的患者达到了病情稳定(SD)。一线治疗中患者中位无进展生存期(PFS)为9.3个月(95%CI,3.5-NR),中位OS尚未达到(95% CI, 7.1-NR)。1年OS率为62% (95% CI, 45%-83%)。
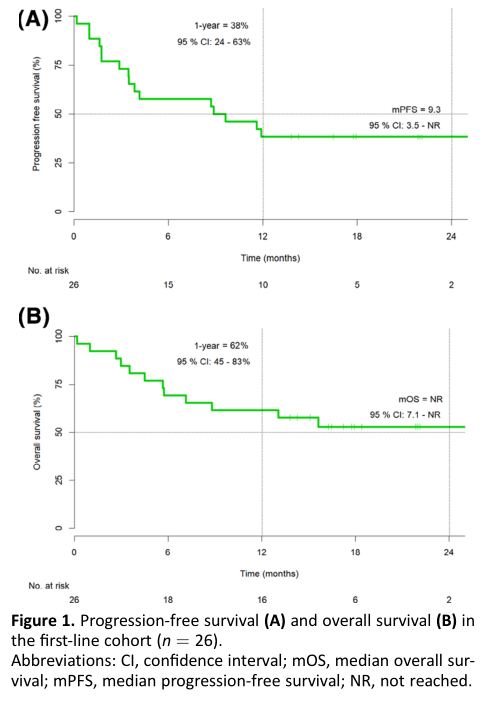
一线治疗的PFS和OS
在二线治疗中,中位随访时间为34.2个月,ORR为25%(10/40) (1例CR和9例PR),另外23%(9/40)的患者达到SD。中位无进展生存期(PFS)为3.5个月(95% CI, 1.9-6.6),中位OS为9.9个月(95% CI, 4.9 -16.1)。1年OS率为35% (95% CI, 23% 53%)。

二线治疗的PFS和OS
66例患者进行安全性评估。79%(52/66)患者出现了治疗相关的不良事件(AEs)。最常见的AEs是疲劳、皮肤疾病、甲状腺功能减退/亢进和肝毒性,每一种都发生在超过15%的患者中。然而,严重的,3级或4级AEs只发生再12%(8/66)的患者。17%(11/66)的患者需要全身皮质类固醇治疗,14%(9/66)的患者因AE而永久停止治疗。在9名因毒性而停止免疫治疗的患者中,2名PR患者有持久的缓解。在停止免疫治疗后,第一例患者的缓解期又延长了5个月,而在数据截止时,第二例患者的缓解期仍超过26个月。无治疗相关死亡记录。
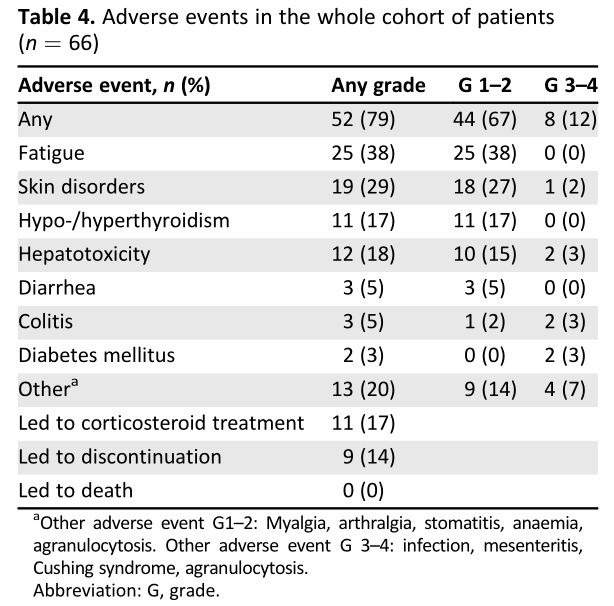
不良事件
综上,这是第一个来自中东欧国家关于免疫治疗在转移性NSCLC患者中疗效的真实世界数据。
原始出处:
M ARIJA I VANOVI, L EA K NEZ , A NA H ERZOG, et al. Immunotherapy for Metastatic Non-Small Cell Lung Cancer: Real-World Data from an Academic Central and Eastern European Center. The Oncologist 2021;25:1–8 www.TheOncologist.com
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Oncol#
61
#非小细胞#
44
#真实世界#
50
#转移性#
44
#GIST#
46
#转移性非小细胞肺癌#
46
谢谢梅斯提供这么好的信息,学到很多
65
谢谢梅斯分享这么多精彩信息
80