梅举:微创左胸小切口多支冠脉搭桥术
2020-12-31 《门诊》杂志 门诊新视野
冠状动脉旁路移植术(Coronary Artery Bypass Graft, CABG)常规使用胸腹正中切口,而这一方法创伤大,术后伤口较大,恢复慢且易产生并发症。
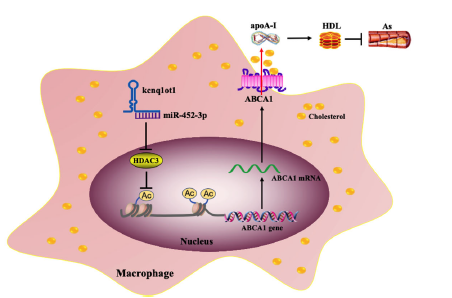
冠状动脉旁路移植术(Coronary Artery Bypass Graft, CABG)常规使用胸腹正中切口,而这一方法创伤大,术后伤口较大,恢复慢且易产生并发症。特别是对于升主动脉粥样硬化、钙化、OPCAB(非体外循环冠状动脉旁路移植术)术中钳夹升主动脉患者,还易出现术后神经系统并发症。通常在在搭桥手术中希望做到全动脉化的目标,这样其术后桥血管的长期通畅率高。运用MIDCAB(微创小切口非体外循环冠脉搭桥术)的方法,创伤小,减少术后并发症,并改善患者术后生存质量。在近期的学术会议上来自上海交通大学医学院附属新华医院(以下简称新华医院)心胸外科的梅举教授,分享了新华医院在微创领域技术的应用与疗效,与诸位专家共勉。
临床资料
自2009年1月~2017年6月,新华医院共实施MIDCAB术92例。采用LIMA-RA(左侧乳内动脉-桡动脉),或LIMA-SV(左侧乳内动脉-大隐静脉)(如>70岁老年患者,或动脉解剖结构不合适的患者)构成的“Y”型复合桥血管治疗冠心病多支病变。
全部患者术前常规行冠状动脉造影,明确冠状动脉病变的诊断。超声心动图检查左心室大小及功能。LVEDD(左室舒张末期内径)为50~56 mm,EF(射血分数)为42~61%。二尖瓣轻度反流27例。这些患者中,合并高血压53例,糖尿病37例,高血脂34例,COPD 18例,肾功能不全15例。
手术技术
手术采用双腔气管插管,单侧右肺通气,并在体表放置体外除颤电极。使用RA为桥血管时,先完成RA的取材。左胸垫高30~40°,经左胸前第四肋间切口。借助于专用撑开器、钛夹钳、电刀,直视下获取LIMA,上至第1肋间,下至第5肋。
完成RA或SV、LIMA取材后,经原切口换一撑开器,纵行切开心包并悬吊,显露靶血管。首先,完成RA或SV与LIMA的端侧吻合,构建LIMA-RA或LIMA-SV “Y”型复合桥血管,并分别观察桥血管的血流量。借助于心脏稳定期,先吻合LIMA-LAD(左侧内乳动脉-左前降支),再采用序贯吻合技术将RA或SV吻合到DIA(对角支)、OM(钝缘支)或PDA(后降支)。
手术结果
在所有行MIDCAB的患者中,91例行LIMA-LAD吻合,1例行LIMA-DIA吻合。靶血管再血管化数目:2支9例,3支75例,4支8例,共275支靶血管再血管化。平均手术时间为185.4±15.7 min(141~213 min)。术后机械通气时间为28.2±34.2 h;ICU时间为3.1±2.4 d;术后住院时间为11.7±4.2 d(7~28 d)。上述指标LIMA-RA组与LIMA-SV组间无明显差异。
LIMA-RA或SV复合桥血管的通畅率方面,术后1年桥血管通畅率:LIMA-RA vs. LIMA-SV为97.6±2.4% vs. 95.7±3.7%(P>0.05),未见明显统计学差异。术后5年桥血管通畅率:LIMA-RA vs. LIMA-SV为93.1±4.7% vs. 80.7±6.6%(P<0.05)。LIMA-SV复合桥血管术后中期通畅率较LIMA-RA复合桥血管术后中期通畅率低,有统计学差异,动脉再血管化效果优于静脉。
围术期全组无死亡。术后随访6~96个月(平均42.1±17.3个月),所有患者均于术后1~8年时,行双源CT或冠脉造影检查,全部患者LIMA-LAD吻合口通畅(100%)。
结 论
LIMA-RA “Y”型复合桥血管可以用于MIDCAB术中多支冠脉搭桥术,手术操作方便,风险小。其中,LIMA-RA用于全动脉化搭桥手术,近、远期通畅率均满意,效果好。手术全程不接触升主动脉,术后卒中发生率低。而LIMA-SV复合桥血管方案也是较好的选择之一。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#搭桥#
46
#冠脉搭桥术#
45
#微创#
33
#搭桥术#
43
#冠脉搭桥#
40