Lancet Neurol:口服脑穿透性BTK抑制剂托莱布替尼治疗复发性多发性硬化症的安全性和有效性?
2021-10-23 Naomii MedSci原创
急性炎症的减少,再加上调节中枢神经系统内免疫反应的可能性,为托莱布替尼在复发性和进展性多发性硬化症患者中进行3期临床试验提供了科学依据。
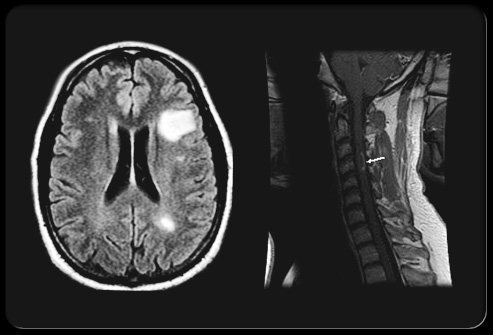
多发性硬化症是一种免疫介导的炎性脱髓鞘疾病,导致轴突丢失、神经疾病和累积的残疾。免疫调节治疗可导致年复发率低至0·10;然而,这些结果不能更多地缓解严重残疾后果。因为现有的治疗主要影响外周适应性免疫。
Bruton酪氨酸激酶是一种非受体酪氨酸激酶,在大多数造血细胞(不包括T细胞和完全分化的浆细胞)中表达,并将特定的细胞表面受体连接到下游的信号通路,将免疫刺激与细胞激活联系起来。它是B淋巴细胞和髓样细胞(包括外周单核细胞或巨噬细胞和中枢神经系统驻留的小胶质细胞)中的关键信号元件。因此,假设抑制Bruton酪氨酸激酶可以减少与造影剂增强相关的急性炎症。抑制中枢神经系统中的Bruton‘s酪氨酸激酶可能对慢性病变和脑膜炎症浸润有好处。这两种类型的病变都包含小胶质细胞、血管周围或脑膜巨噬细胞以及B系细胞,已证明对治疗干预具有抵抗力。因此,靶向中枢神经系统内外的B细胞和髓样细胞在神经炎症和脱髓鞘方面可能比目前的疾病修饰疗法有更大甚至可能是协同效果。
托莱布替尼是一种口服的小分子,它不可逆地与布鲁顿的酪氨酸激酶结合并抑制其活性。第一阶段研究表明,脑脊液中药物的浓度与药物有关。例如,在健康志愿者中单次口服120 mg托莱布替尼,在2h后脑脊液中的平均浓度为4.1nM,这是基于细胞分析的治疗相关暴露。近日,有研究人员试图确定托莱布替尼与复发性多发性硬化症患者新的活动性脑MRI病灶减少之间的剂量-反应关系。
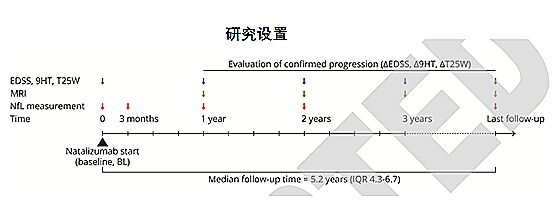
研究人员在欧洲和北美的10个国家的40个中心(学术场所、专科诊所和普通神经病学中心)进行了为期16周的2b期随机、双盲、安慰剂对照、交叉剂量发现试验。符合条件的参与者是18-55岁的成年人,他们被诊断为复发性多发性硬化症(复发-缓解型或复发性继发性进行性多发性硬化症),并符合以下一项或多项标准:在过去一年内至少复发一次,在过去两年内至少复发两次,或在筛查前6个月内至少一次活跃的增强钆的脑损伤。排除标准包括诊断为原发性进行性多发性硬化症或诊断为无复发的继发性进行性多发性硬化症。研究使用两步随机过程将符合条件的参与者(1:1)随机分配到两个队列中,然后进一步将每个队列中的参与者(1:1:1:1)随机分配到四个托莱布替尼剂量组(每天一次口服托莱布替尼5,15,30和60毫克)。第1组服用托莱布替尼12周,然后配对安慰剂(即外观相同的片剂)4周;第2组服用4周的安慰剂,然后服用12周的托莱布替尼。参与者和研究人员被掩盖了剂量和托莱布替尼-安慰剂给药顺序;研究人员、研究团队成员和研究参与者无法获得未掩盖的数据。MRI扫描在筛查时进行,每隔4周扫描一次,超过16周。主要疗效终点是在接受托莱布替尼治疗12周(队列1在第12周评估,队列2在第16周评估)后,相对于4周前的扫描,在扫描中发现的新的钆增强病变的数量,并与在队列2的安慰剂磨合期4周内累积的病变进行比较。疗效数据在一个改良的意向治疗人群中进行了分析,采用两步多重比较程序和建模分析。对所有接受了至少一剂研究药物的参与者进行了安全性评估。该试验已在ClinicalTrials.gov(NCT03889639)、EudraCT(2018年-003927-12年)和世卫组织(U111112200572)注册,并已完成。
- 在2019年5月14日至2020年1月2日期间,共招募并随机分配了130名参与者服用托莱布替尼:33至5毫克、32至15毫克、33至30毫克和32至60毫克。129例(99%)完成治疗方案,126例进入初步分析。
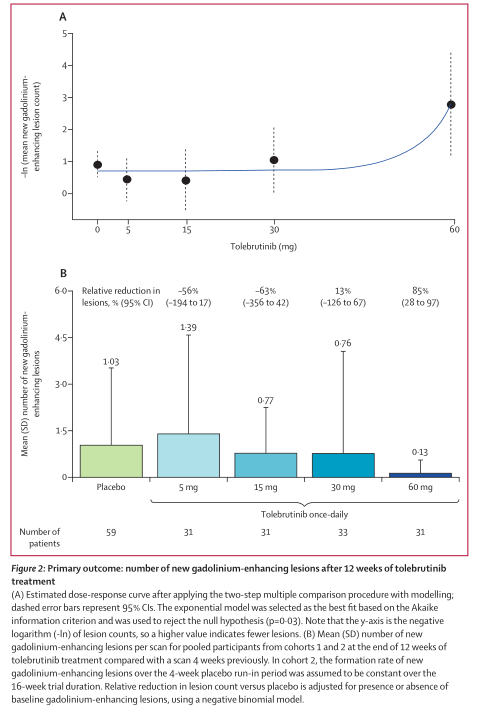
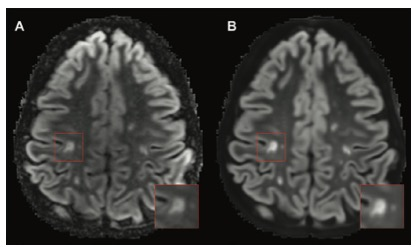
- 在治疗第12周,新的钆强化病灶数目呈剂量依赖性减少(平均每位患者的[SD]病灶:安慰剂,1·03[2·50];5 mg,1·39[3·20];15 mg,0·77[1·48];30 mg,0·76[3·31];60 mg,0·13[0·43];p=0·03)。
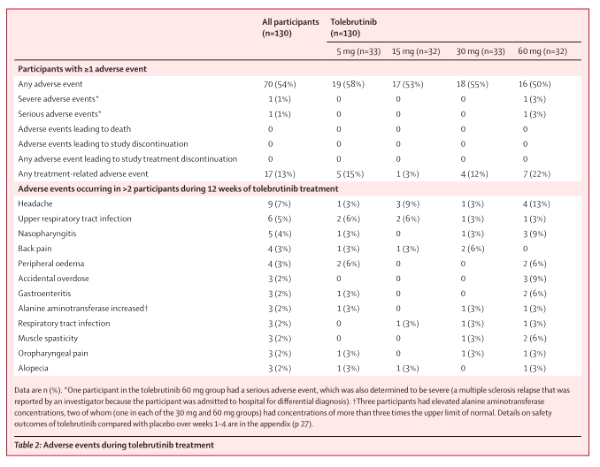
- 报告了1起严重的不良事件(60毫克组中有1名患者因多发性硬化症复发而入院治疗)。托莱布替尼治疗期间最常见的非严重不良反应是头痛(5毫克组33人中有1人[3%]头痛;15毫克组32人中有3人[9%];30毫克组33人中有1人[3%];60毫克组32人中有4人[13%])。
- 没有发生与安全相关的中止或与治疗相关的死亡。
托莱布替尼治疗12周后,钆增强的新病灶呈剂量依赖性减少,其中60毫克剂量最有效,且药物耐受性良好。急性炎症的减少,再加上调节中枢神经系统内免疫反应的可能性,为托莱布替尼在复发性和进展性多发性硬化症患者中进行3期临床试验提供了科学依据。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#抑制剂#
26
#复发性多发性硬化症#
39
#安全性和有效性#
42
#Neurol#
35
#Lancet#
33
#复发性#
31
#硬化症#
26
#多发性#
28
#BTK抑制剂#
38
#BTK#
28