Rheumatol Int:儿童慢性非细菌性骨髓炎:多中心病例系列报道
2020-12-03 MedSci原创 MedSci原创
慢性非细菌性骨髓炎(CNO)是一种原发性自体炎性骨病,多见于儿童,其特点是在没有感染性病因的情况下出现骨质炎症病变。拉丁美洲对该病的资料很少。一项回顾性研究评估了拉丁美洲儿童CNO患者的人口学、临床、
慢性非细菌性骨髓炎(CNO)是一种原发性自体炎性骨病,多见于儿童,其特点是在没有感染性病因的情况下出现骨质炎症病变。拉丁美洲对该病的资料很少。一项回顾性研究评估了拉丁美洲儿童CNO患者的人口学、临床、实验室、影像学、组织病理学特征和治疗反应。研究结果已在线发表于Rheumatol Int。
研究人员回顾了2007年至2019年期间在智利圣地亚哥三个三级中心诊断的19名CNO患者的临床记录。
患儿的发病的中位年龄为10岁,47%为女性患儿。诊断的中位延迟时间为12个月。所有患者都有复发性多灶性疾病的模式。37%的患者抗核抗体阳性,16%的患者HLA-B27阳性。21%的患者出现关节炎或其他风湿病合并症,但是没有观察到患者出现银屑病、炎症性肠病(IBD)或掌跖脓疱病(PPP)。
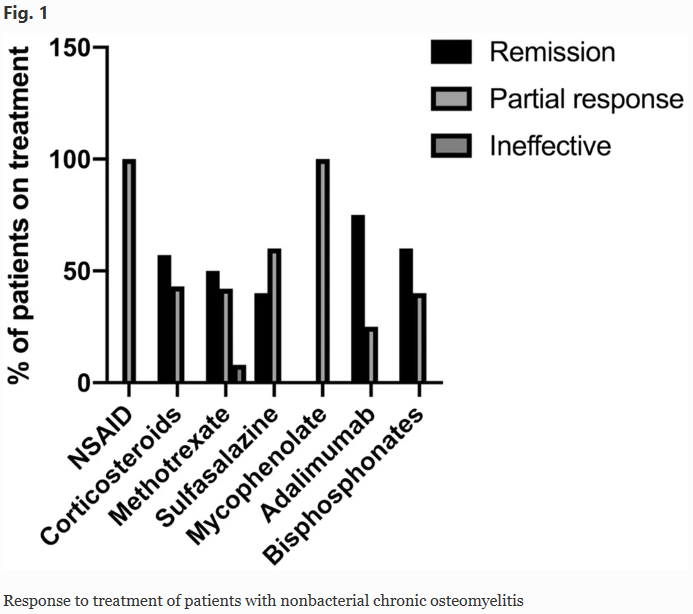
18名患者接受了非甾体类抗炎药物治疗,部分患儿对治疗有反应。12名患者接受甲氨蝶呤治疗,其中一半患儿同时接受类固醇治疗,达到50%的缓解率。在接受双膦酸盐治疗的5名患者中,60%的患儿缓解。接受阿达木单抗治疗的4名患者合并关节炎,75%的患者达到缓解。
综上所述,该回顾性研究结果表明,该研究所纳入的CNO患儿均出现多灶性病变,常并发自身免疫性疾病,包括关节炎,但没有观察到并发银屑病、IBD或PPP。
原始出处:
Sara Concha, Alfonso Hernández-Ojeda, et al., Chronic nonbacterial osteomyelitis in children: a multicenter case series. Rheumatol Int. 2020 Jan;40(1):115-120. doi: 10.1007/s00296-019-04400-x.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












很有用
73
#多中心#
36
#骨髓炎#
58
看了
143
这是新的一天继续学习了
102
不错
98