BMC MED:LDL-C达标就不会中风?错!没有进行调脂治疗仍可能有高的卒中风险!
2022-07-10 MedSci原创 MedSci原创
有证据表明,低密度脂蛋白胆固醇(LDL-C)浓度很低的个体发生中风的风险仍然很高。
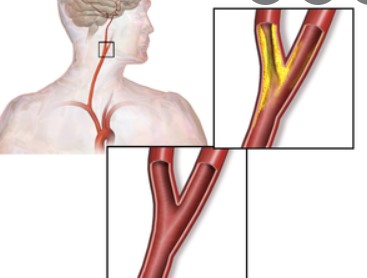
有证据表明,低密度脂蛋白胆固醇(LDL-C)浓度很低的个体发生中风的风险仍然很高。来自我国的学者试图利用机器学习方法中的生存条件推理树,对LDL-C浓度<70 mg/dL(3.85mmol/L)的中国参与者的中风预测性风险因素进行优先排序。结果发表在BMC MEDICINE杂志上。
训练数据集包括9327名LDL-C浓度<70 mg/dL、无心血管疾病且未使用调脂药物的开滦一期研究人员(N = 101510)。在第二个中国队列中检查了该算法的有效性,该队列包括开滦二期研究中1753名LDL-C浓度<70 mg/dL的参与者(N = 35856)。
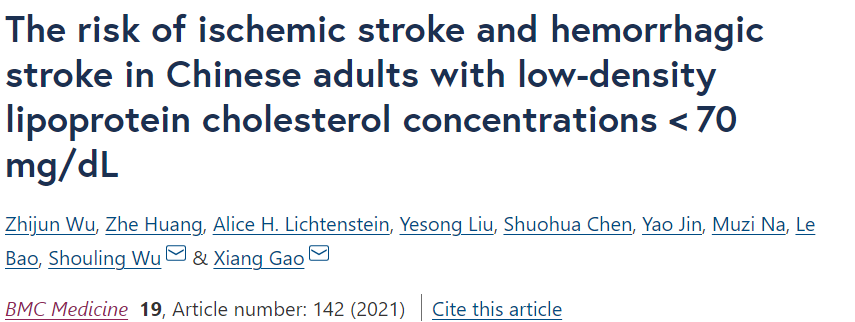
结果显示,在平均8.5-9.0年的随访期间,研究人员在训练数据集中发现388例缺血性卒中和145例出血性卒中,在验证数据集中发现20例缺血性卒中和8例出血性卒中。在15个检查的预测因子中,血压控制不佳和LDL-C浓度很低(≤40 mg/dL)是缺血性卒中风险和出血性卒中风险的最高层次预测因子。
相对于最低风险组(存在这些因素的0-1)的患者,存在2-3个上述风险因素为特征的群体与较高的缺血性卒中风险有关(训练集HR=7.03;95%CI 5.01-9.85;验证集HR=4.68,95%CI 1. 58-13.9)和出血性卒中(训练集HR=3.94,95%CI 2.54-6.11;验证集HR=4.73,95%CI 0.81-27.6)。累积平均LDL-C浓度与卒中风险之间存在线性关系。调整年龄、高血压状态和其他协变量后,与LDL-C浓度为55-70 mg/dL相比,LDL-C浓度≤40 mg/dL与缺血性卒中(HR= 2.07, 95%CI 1.53, 2.80)和出血性卒中(HR= 2.70, 95%CI 1.70, 4.30)风险增加明显相关。
综上,低密度脂蛋白胆固醇浓度极低的人,如果以前没有进行调脂治疗,仍可能有高的卒中风险。
参考文献:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#BMC#
46
#卒中风险#
37
#LDL#
0
#Med#
28
#调脂治疗#
44
#调脂#
36