Nat Cell Biol:三阴性乳腺癌需要对“症”下药
2020-04-26 佚名 生物通
宾夕法尼亚大学的Rumela Chakrabarti领导的研究发现了一种导致三阴性乳腺癌进展和扩散的分子途径。
宾夕法尼亚大学的Rumela Chakrabarti领导的研究发现了一种导致三阴性乳腺癌进展和扩散的分子途径。

免疫疗法彻底改变了各种癌症治疗,但三阴性乳腺癌(TNBC)只有不到20%的患者对免疫疗法有反应。
“为什么其他人没有回应?”宾夕法尼亚大学兽医学院助理教授Rumela Chakrabarti说。
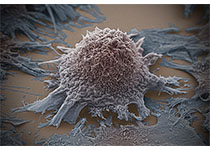
在《Nature Cell Biology》的一篇新论文中,Chakrabarti和他的同事阐明了这个问题的分子机理。他们发现了一种针对TNBC患者的可靶向治疗的信号通路。利用模仿人类疾病关键特征的疾病小鼠模型,他们证明失活蛋白质ELF5会促进另一种蛋白质干扰素γ受体1的活性。稳定的干扰素γ受体1导致激活的干扰素γ信号传导,进而导致肿瘤侵袭性和扩散增加,这条途径可以通过阻断干扰素γ信号传导加以缓解。
“这非常奇怪,”Chakrabarti说。“因为干扰素γ常常对癌症有保护作用,而且通常作为癌症治疗给一些患者。它在某些癌症类型中工作良好,但对于三阴性乳腺癌的特定亚型,我们发现阻断干扰素γ反而可能是患者的最佳策略。”
Chakrabarti对ELF5蛋白的生物学有着很深的了解。十多年前,她作为纽约州立大学布法罗分校(State University of New York at Buffalo)的博士后研究员就开始研究它,发现它的正常功能是支持怀孕和哺乳。2012年,她和同事在《Chakrabarti》杂志上发表了一份报告,显示ELF5可以抑制一个关键的转变,这种转变是为了使乳腺癌扩散。
然而,早期的研究并没有特别关注TNBC,部分原因是科学家缺乏有效的小鼠模型。在三年的时间里,Chakrabarti的团队开发了一个临床前TNBC模型,该模型概括了该疾病的两个特征:扩散倾向和伴随肿瘤生长的免疫细胞的涌入。
在目前的研究中,研究人员发现,当这些TNBC小鼠的肿瘤也失去了ELF5蛋白的功能时,它们的发病过程与人类患者的更为相似。“失去ELF5使这种疾病具有很强的转移性和侵略性。”
为了阐明导致更危险的TNBC形成的分子机制,Chakrabarti和同事检测了肿瘤细胞中表达的RNA,这些肿瘤细胞失去了ELF5的表达。他们发现干扰素γ途径的活性增加,他们相信,这是由于该蛋白受体的表达增加所致。这种缺失也导致了中性粒细胞的聚集,中性粒细胞是一种免疫细胞,具有免疫抑制功能。相反,保留ELF5的正常乳腺细胞具有低水平的干扰素γ信号。
使用抗干扰素γ受体1的抗体或通过基因操纵肿瘤细胞表达较低水平的受体来阻断这一信号,导致肿瘤生长和扩散更加缓慢。
最后,为了确定小鼠模型中的这些发现是否与人类相关,研究小组研究了患者的基因和蛋白质数据,以确定他们的ELF5水平和干扰素γ受体表达。他们观察到,ELF5水平较低和受体水平较高的患者情况较差,癌症往往在身体周围扩散得更快。
Chakrabarti说,使用干扰素γ和免疫疗法治疗癌症患者的临床医生应该仔细考虑这些发现。如果某人的ELF5水平较低,除了进行免疫治疗外,还应给予干扰素γ信号阻断治疗。
在未来的工作中,Chakrabarti团队将深入研究TNBC的免疫学,研究不同免疫细胞在推动癌症转移和侵袭中的作用。他们还希望了解他们在TNBC中发现的干扰素γ信号是否适用于其他类型的肿瘤,如肾癌和卵巢癌。
原始出处:Singh S, Kumar S, Srivastava RK, et al. Loss of ELF5–FBXW7 stabilizes IFNGR1 to promote the growth and metastasis of triple-negative breast cancer through interferon-γ signalling. Nat Cell Biol. 2020 Apr 13.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Nat#
34
#Biol#
29
#Bio#
36
#阴性乳腺癌#
27
#Cell#
33
#CEL#
30
#三阴性#
23
学习了,很好的分享
91